Treating Acute Agitation with Ketamine in the Emergency Department
Critical Care / Resuscitation, Psychiatric and Behaviour
Context
- Acute agitation is a common ED presentation that most often stems from intoxication, decompensated psychiatric illness, or an acute medical illness.1-6
- These patients require rapid control of their behaviour to prevent further deterioration of their illness, avoid harm to themselves and staff, and allow for safe assessment.1,3-9
Recommended Treatment
When is chemical sedation necessary?
- When first-line interventions such as verbal de-escalation or oral medications are ineffective patients may require physical and chemical restraints for behavioural control.2,5,9-12
- Physical restraints should never be used without sedation as they can cause direct physical injury, and worsen metabolic decompensation.4,7,10
- Traditional treatment has relied on benzodiazepines and antipsychotics,1,6,13 but these are slow, produce a variable clinical response, and can result in complications such as respiratory depression, hypoxemia, unplanned airway interventions, cardiac dysrhythmia, and movement disorders.1,3,5-7,9,11,12,14
What is Ketamine, and should we use it?
- Ketamine has demonstrated both safety and efficacy when used as a first-line option for patients who require rapid behavioural control.1-3,5,6,9,11,12,14
- It is a non-competitive NMDA-receptor antagonist that blocks glutamate and causes a dissociative state.6,15
- Once dissociation is achieved, additional doses do not lead to deeper sedation or reduce respiratory drive.3,5,6,14,15 It has been shown to preserve cardiovascular and respiratory reflexes, and rarely causes dysrhythmias.1,3-7,9,15
- Ketamine’s weak sympathomimetic action causes temporary increases in HR and BP, but these effects are not of concern.3,5-7,12
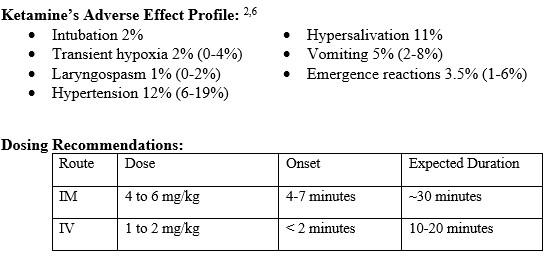
- For repeat dosing or use as a rescue medication, dose reductions of 50% are recommended with time intervals of 5-10minutes for IV and 10-25min for IM.
- Dosing reductions may also need to be considered for severely ill patients who are catecholamine deplete (i.e., septic shock), as ketamine can induce hypotension in these populations.17,18
Other considerations:
1) Patients given ketamine should have full cardio-respiratory monitoring to allow for quick recognition or intervention of adverse events.1,6,9
2 When combined with other substances the effects of ketamine are unclear, and its unknown whether there is an increased risk for a hypoxic event.5
3) Ketamine is not thought to cause significant changes in cerebral perfusion pressure.7
Criteria For Hospital Admission
Disposition and Consultation:10,19
- Organic illnesses must be ruled out.
- Patients > 40 yo with new psychiatric symptoms are more likely to have an organic cause.
- Elderly patients are at higher risk for organic delirium.
- Patients with a history of drug or alcohol abuse may exhibit violent behavior as part of an intoxication or withdrawal syndrome.
- If the agitation is related to substances or intoxication, the patient should be observed until they can participate in a psychiatric interview.
- Violent behavior not due to an underlying medical condition or drug intoxication, should receive psychiatric evaluation.
- Patients at imminent risk to themselves or others should be held involuntarily for psychiatric evaluation.
Criteria For Transfer To Another Facility
Indications:
If the patient does not clear, or additional consultation and/or medical workup (i.e., neuroimaging) are required beyond the capabilities of the facility, then the patient should be transferred to a center with a higher level of care by a team capable of advanced airway intervention.
Criteria For Close Observation And/or Consult
Initial Resuscitation:10-12
- Severely agitated patients should be placed in the resuscitation room.
- Assess for and treat hypoxia, hyperthermia, hypoglycemia, and hypovolemia; and consider acidosis, hyperkalemia, and CNS lesions.
- Vital signs q5min for at least the first 30 minutes.
Monitoring of the physically restrained patient:10-12
- The patient should be reassessed frequently for signs of altered respiratory mechanics, neurovascular compromise, or injuries related to the restraints.
- Physical restraints should only be used as a bridge to chemical sedation.
Monitoring of the chemically restrained patient:
- Patients sedated with ketamine should have full cardiopulmonary monitoring and be treated 1:1 like a procedural sedation.1,6,9-12
- Vital signs, including blood glucose, must be obtained.
- Combative patients who are sedated and later deteriorate usually do so because of an unrecognized infection, trauma, toxidrome, or neurologic cause.10
Criteria For Safe Discharge Home
Discharge may be appropriate if: 10
- The violent behavior was caused by a temporary syndrome
- Medical and psychiatric evaluations are normal with no required intervention.
- The patient is no longer a risk to themselves or others.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
A 2018 systemic review6 highlighted how the studies analyzing ketamine’s efficacy and safety were observational, retrospective, or case series; and there was a lack of quality evidence. Since then, three RCTs 1,2,5 have been able to confirm ketamine’s efficacy and significantly faster time to sedation. While these smaller RCTs were able to prove efficacy, there were not powered to prove safety.
Related Information
Reference List
Barbic D, Andolfatto G, Grunau B, Scheuermeyer FX, Macewan B, Qian H, Wong H, Barbic SP, Honer WG. Rapid Agitation Control With Ketamine in the Emergency Department: A Blinded, Randomized Controlled Trial. Ann Emerg Med. 2021 Dec;78(6):788-795. doi: 10.1016/j.annemergmed.2021.05.023. Epub 2021 Aug 2. PMID: 34353650.
Heydari F, Gholamian A, Zamani M, Majidinejad S. Effect of Intramuscular Ketamine versus Haloperidol on Short-Term Control of Severe Agitated Patients in Emergency Department; A Randomized Clinical Trial. Bull Emerg Trauma. 2018 Oct;6(4):292-299. doi: 10.29252/beat-060404. PMID: 30402516; PMCID: PMC6215072.
Hopper AB, Vilke GM, Castillo EM, Campillo A, Davie T, Wilson MP. Ketamine use for acute agitation in the emergency department. J Emerg Med. 2015 Jun;48(6):712-9. doi: 10.1016/j.jemermed.2015.02.019. Epub 2015 Apr 2. PMID: 25843924.
Li M, Martinelli AN, Oliver WD, Wilkerson RG. Evaluation of Ketamine for Excited Delirium Syndrome in the Adult Emergency Department. J Emerg Med. 2019 Nov 14:S0736-4679(19)30802-9. doi: 10.1016/j.jemermed.2019.09.019. Epub ahead of print. PMID: 31735659.
Lin J, Figuerado Y, Montgomery A, Lee J, Cannis M, Norton VC, Calvo R, Sikand H. Efficacy of ketamine for initial control of acute agitation in the emergency department: A randomized study. Am J Emerg Med. 2021 Jun;44:306-311. doi: 10.1016/j.ajem.2020.04.013. Epub 2020 Apr 11. PMID: 32340820.
Mankowitz SL, Regenberg P, Kaldan J, Cole JB. Ketamine for Rapid Sedation of Agitated Patients in the Prehospital and Emergency Department Settings: A Systematic Review and Proportional Meta-Analysis. J Emerg Med. 2018 Nov;55(5):670-681. doi: 10.1016/j.jemermed.2018.07.017. Epub 2018 Sep 7. PMID: 30197153.
Kowalski JM, Kopec KT, Lavelle J, Osterhoudt K. A Novel Agent for Management of Agitated Delirium: A Case 8Series of Ketamine Utilization in the Pediatric Emergency Department. Pediatr Emerg Care. 2017 Sep;33(9):e58-e62. doi: 10.1097/PEC.0000000000000578. PMID: 26466151.
O’Brien ME, Fuh L, Raja AS, White BA, Yun BJ, Hayes BD. Reduced-dose intramuscular ketamine for severe agitation in an academic emergency department. Clin Toxicol (Phila). 2020 Apr;58(4):294-298. doi: 10.1080/15563650.2019.1643468. Epub 2019 Jul 23. PMID: 31335216.
Riddell J, Tran A, Bengiamin R, Hendey GW, Armenian P. Ketamine as a first-line treatment for severely agitated emergency department patients. Am J Emerg Med. 2017 Jul;35(7):1000-1004. doi: 10.1016/j.ajem.2017.02.026. Epub 2017 Feb 13. PMID: 28237385.
Moore GP., Pfaff JA. Assessment and emergency management of the acutely agitated or violent adult. In J. Grayzel (Ed.), UptoDate, 2021 Accessed Dec 10, 2021. Available from: https://www.uptodate.com/contents/assessment-and-emergency-management-of-the-acutely-agitated-or-violent-adult#H16
Weingart S, Strayer R. The Decision to use Ketamine – Disruptive and Dangerous. Ep 279. EMCrit Blog. August 9, 2020. Accessed November 20th 2021. Available from: https://emcrit.org/emcrit/dangerous-and-disruptive/
Helman, A, Strayer, R, Thompson, M. Emergency Management of the Agitated Patient. Emergency Medicine Cases. September, 2018. https://emergencymedicinecases.com/emergency-management-agitated-patient/. Accessed November 15, 2021
Isbister GK, Calver LA, Downes MA, Page CB. Ketamine as Rescue Treatment for Difficult-to-Sedate Severe Acute Behavioral Disturbance in the Emergency Department. Ann Emerg Med. 2016 May;67(5):581-587.e1. doi: 10.1016/j.annemergmed.2015.11.028. Epub 2016 Feb 18. PMID: 26899459.
Korczak V, Kirby A, Gunja N. Chemical agents for the sedation of agitated patients in the ED: a systematic review. Am J Emerg Med. 2016 Dec;34(12):2426-2431. doi: 10.1016/j.ajem.2016.09.025. Epub 2016 Sep 16. PMID: 27707527.
Mo H, Campbell MJ, Fertel BS, Lam SW, Wells EJ, Casserly E, Meldon SW. Ketamine Safety and Use in the Emergency Department for Pain and Agitation/Delirium: A Health System Experience. West J Emerg Med. 2020 Jan 27;21(2):272-281. doi: 10.5811/westjem.2019.10.43067. PMID: 31999250; PMCID: PMC7081852.
Lexicomp. Ketamine: Drug information. [cited Nov 15, 2021]. In: UpToDate. Waltham, MA: UpToDate Inc. Available from: https://www.uptodate.com/contents/ketamine-drug-information
Mohr NM, Pape SG, Runde D, Kaji AH, Walls RM, Brown CA 3rd. Etomidate Use Is Associated With Less Hypotension Than Ketamine for Emergency Department Sepsis Intubations: A NEAR Cohort Study. Acad Emerg Med. 2020 Nov;27(11):1140-1149. doi: 10.1111/acem.14070. Epub 2020 Jul 20. PMID: 32602974.
April MD, Arana A, Schauer SG, Davis WT, Oliver JJ, Fantegrossi A, Summers SM, Maddry JK, Walls RM, Brown CA 3rd; NEAR Investigators. Ketamine Versus Etomidate and Peri-intubation Hypotension: A National Emergency Airway Registry Study. Acad Emerg Med. 2020 Nov;27(11):1106-1115. doi: 10.1111/acem.14063. Epub 2020 Jul 18. PMID: 32592205
American College of Emergency Physicians. Emergency medicine practice management & health policy: psychiatric patients in the emergency department. Heaton HA. Accessed Dec 1, 2021. https://www.acep.org/how-we-serve/sections/emergency- medicine-practice-management–health-policy/news/september- 2015/psychiatric-patients-in-the-emergency-department/.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 13, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.