Postpartum Psychosis – Diagnostic and Therapeutic
Pregnancy, Psychiatric and Behaviour, Special Populations
Context
- Postpartum psychosis is a true psychiatric and obstetrical emergency with an incidence of 0.3 to 2 per 1,000 live births.
- Early recognition and adequate treatment is critical.
- Typically requires inpatient management and may require non-voluntary admission.
- Associated with increased risk of suicide and infanticide.
- Approximately 33% of presentations will be a woman’s first psychiatric presentation.
Diagnostic Process
Identify Risk Factors:
- Personal history of bipolar disorder (20-30% of presentations).
- Primiparity.
- Family history of bipolar disorder or postpartum psychosis.
- Sleep disturbance.
Presentation:
- Onset typically within the first 2 weeks postpartum (within hours to 4 weeks).
- Onset typically sudden but may have waxing and waning of symptoms.
- Poor insight into symptoms and severity.
- Abnormal thought content may include bizarre and persecutory delusions.
- May present with disorganization, disorientation.
- May present with predominant manic/psychotic features, predominant depression/anxiety/irritability, or mixed/atypical .
- May present with ego-syntonic infanticidal thoughts (i.e. believing the baby would be better off dead). This contrasts with ego-dystonic thoughts of harming the baby in postpartum OCD.
- May present with suicidal ideation.
Differential Diagnosis:
- Baby blues, postpartum depression, generalized anxiety disorder, obsessive-compulsive disorder, auto-immune encephalitis, Sheehan’s syndrome, neuropsychiatric symptom of lupus, postpartum thyroiditis, intoxication, medication reaction.
Diagnostic Screening Tools:
- None validated.
- Screening questions should include: psychiatric history, presence of delusions, suicidal ideation/risk assessment, infanticidal ideation/risk assessment, substance use history, family history of bipolar disorder or postpartum psychosis.
Infanticide Risk Assessment Screening (taken from BC Best Practice Guidelines for Mental Health Disorders in the Perinatal Period, see full document for further details):
- Consider beginning the conversation with a statement such as: “Sometimes after birth, women have thoughts about harming their babies” before proceeding with direct questions.
- Have you had any thoughts of harming your baby?
- Do you have thoughts of harming yourself and the baby?
- Have you ever attempted to harm your baby?
- Do you think your baby would be better off dead?
Diagnostic Considerations:
- In the emergency department, care providers should seek collateral information as insight in this condition is poor.
- Urgent psychiatric consultation prior to disposition in the emergency department is required.
- If there is concern about the safety of the infant or children at home, there is a duty to report to MCFD (phone 310-1234, no area code required).
Recommended Treatment
Recommended Treatment in the Emergency Department:
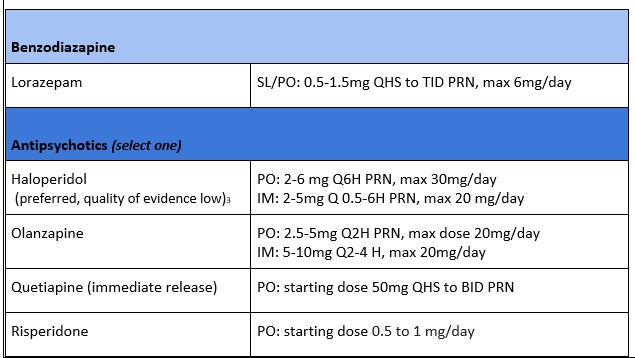
- Benzodiazepine may be considered for monotherapy while awaiting psychiatric assessment in the emergency department.
- Concurrent use of benzodiazepines and an antipsychotic is typical for acute treatment of manic and psychotic symptoms.
- If this is a recurrence, consider what agent has been helpful for this patient in the past.
- Drugs listed below are considered Lactation Risk L3 or L2 (“moderately safe” or “safer”).
Medical Management of Acute Postpartum Psychosis in the Emergency Department:
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
- Medical management of postpartum psychosis quality of evidence: Low.
Prospective studies are limited in number, limited in geographic/sociologic variability, have small sample sizes, and do not include randomized or blinded trials of treatment protocols.
Related Information
Reference List
Osborne L. M. (2018). Recognizing and Managing Postpartum Psychosis: A Clinical Guide for Obstetric Providers. Obstetrics and gynecology clinics of North America, 45(3), 455–468.
Beerink, V. et al. (2015). Treatment of Psychosis and Mania in the Postpartum Period. American Journal of Psychiatry. 2015 Feb 1;172(2):115-23.
Rommel, A.S. et al. (2021). Long-term outcome of postpartum psychosis: a prospective clinical cohort study in 106 women. International Journal of Bipolar Disorder, 31(9).
Best Practice Guidelines for Mental Health Disorders in the Perinatal Period, BC Reproductive Mental Health Program and Perinatal Services BC, March 2014. http://www.perinatalservicesbc.ca/Documents/Guidelines-Standards/Maternal/MentalHealthDisordersGuideline.pdf
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 31, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.