Hypertensive Emergencies
Cardiovascular
Context
- Hypertensive Emergency = a collection of syndromes whereby an acute elevation of BP causes acute target organ damage. Requires immediate treatment.
- Hypertensive Emergencies represent approximately 0.1%-1% of patients. 1-3% with hypertension have a hypertensive emergency in their lifetime.
- In-hospital death is 2.5% (~4.6% when admitted to CCU).
- If untreated, median survival is 10.4 months and 1-year death rate >79%.
- Hypertensive Urgencies or Severe Asymptomatic Hypertension = Systolic BP >180 or Diastolic BP >120 mmHg without target organ damage. Optimal timeframe for initiating treatment is < 1 week to up to 3 months.
* This clinical summary will not address rare conditions such as pheochromocytoma.
What represents acute target organ damage?
- Acute heart failure/pulmonary edema (22-30%).
- Acute coronary syndrome (18-25%).
- Aortic dissection (3.5-8%).
- Hypertensive encephalopathy (2.6-16%).
- Acute ischemic stroke (24%).
- Intracranial hemorrhage (4.5-15%).
- Acute kidney injury (0.5%).
- Hypertensive retinopathy.
- Eclampsia/Pre-eclampsia (up to 6 weeks post-delivery).
Note: Headache (non-pregnant) or epistaxis are not target organ damage
Clinical Endpoint
- Hypertensive Emergency patients should be admitted to ICU.
- Immediate BP reduction and hospitalization not indicated for Hypertensive Urgency/Severe Asymptomatic Hypertension.
Diagnostic Process
Historical features
- Missed anti-hypertensives.
- Recently started or discontinued medications (eg. clonidine).
- Recreational drugs (eg. cocaine, amphetamines, phencyclidine).
- Disease processes (eg. hyperaldosteronism, thyroid storm, autonomic dysreflexia).
- Physiological processes (eg. Pain).
- # weeks gestation if pregnant, or delivery date.
- Baseline BP if known and comorbid medical conditions.
- Previous hypertensive emergencies/pre-existing target organ damage.
Most patients: CBC, Electrolytes, BUN, Creatinine, Glucose, B-HCG.
- Acute Coronary Syndrome
- Chest pain/anginal equivalents, dyspnea, increased fatigue, vomiting.
- Murmur or S3 – possible papillary dysfunction, diaphoretic.
- ECG, troponin (+ repeat if indicated by site/guidelines).
- Aortic Dissection
- Chest pain/anginal equivalents, back/abdo pain, neurological deficits, syncope.
- Unequal BP (>20 mmHg) in extremities, pulse differential, focal neurological deficits.
- CXR, POCUS – for dissection flap,
- CT Chest with contrast,
- Troponin – coronary dissection.
- Acute heart failure/pulmonary edema
- Dyspnea, increased fatigue, orthopnea, cough.
- Murmur or S3, edema, crackles on auscultation, elevated JVP, hypoxia.
- CXR, ECG, POCUS – myocardial function, TSH, Liver enzymes.
-
- Ischemic stroke, intracranial hemorrhage, hypertensive encephalopathy
- Altered mental status, neurological deficits focal and non-focal, vomiting (raised ICP).
- CN abnormalities, power/sensation/reflex/cerebellar deficits.
- INR/PTT, CT Head with + without contrast.
- Ischemic stroke, intracranial hemorrhage, hypertensive encephalopathy
- Pregnancy
- Pre-eclampsia:
- Headache, visual disturbance, abdominal pain (RUQ).
- RUQ pain, edema.
- B-HCG, CBC, Creatinine, Liver enzymes for HELLP syndrome, urine dip – for protein.
- Eclampsia:
- Seizures.
- Pre-eclampsia:
- Acute kidney injury
- Decreased urine output.
- Edema.
- Creatinine.
- Sympathomimetics
- Various presentations, chest pain – cocaine vasospasm, acute heart failure.
- Hyperthermic.
- Urine toxicology – cocaine, amphetamines, phencyclidine.
- Hypertensive retinopathy
- Blurred vision or visual field defects.
- Fundoscopy flame hemorrhages and exudates.
Treatment Goals
- Elevated BP without target organ damage (Hypertensive Urgency/Severe Asymptomatic Hypertension) requires no emergent treatment.
- For Hypertensive Emergencies manage target organ damage/reduce complications.
- No RCTs show improved morbidity/mortality benefits from treatment but expert consensus and guidelines suggest high likelihood of benefit.
Treatment Principles
- Monitored bed, regular BP monitoring.
- 1st hour: reduce SBP (or MAP) 20-25% (ideally within minutes for eclampsia and aortic dissections).
- 2-6 hrs: subsequent reduction to <160 mmHg Systolic and <100-110 mmHg Diastolic.
- 24-48 hrs: Return to baseline BP if known, <140/90 if unknown (low evidence).
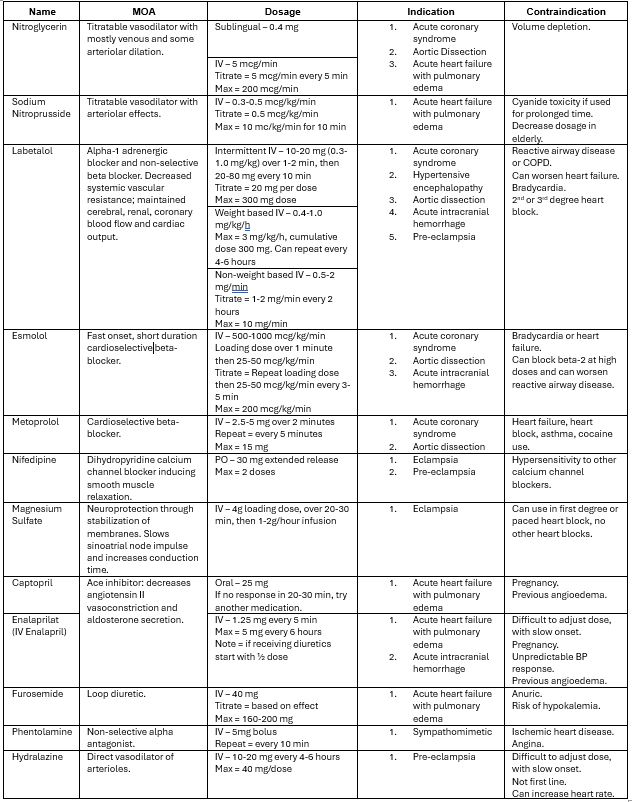
Antihypertensive Medications:
- No single antihypertensive agent is recommended.
- Use intravenous medications.
- Rapid-acting sublingual or oral medications (nitroglycerin spray, captopril) can be useful while setting up infusion/lack of IV access.
Specific Considerations
Acute LV Failure with Pulmonary Edema
- Nitroglycerin OR Sodium Nitroprusside.
- Furosemide.
- Avoid hydralazine (increased cardiac work) and beta-blockers (decreased cardiac contractility).
Acute Coronary Syndromes
- Nitroglycerin OR Labetalol OR Esmolol.
- Avoid hydralazine (increased cardiac work).
Aortic Dissection
- Rapid HR reduction in first 10 minutes to <60.
- BP reduction to <120 mmHg in first 20 min, discussion with ICU on need for arterial line.
- Labetalol OR Esmolol OR Metoprolol OR Nitroglycerin OR Sodium Nitroprusside.
Eclampsia/Pre-eclampsia
- Magnesium sulfate in eclampsia.
- Nifedipine OR Labetalol OR Hydralazine OR Methyldopa in pre-eclampsia.
Hypertensive Encephalopathy
- Diagnosis of exclusion after ruling out intracranial pathology.
- Labetalol OR Hydralazine.
- Avoid sodium nitroprusside if suspected ICP due to intracerebral shunting.
Acute Ischemic Stroke
- Higher MAP essential to perfusion. BP should not be lowered acutely except at extremes (some clinicians use >220/120). Gradual BP reduction should occur.
- Thrombolysis contraindicated with extreme hypertension due to risk of bleeding. Lower BP to <185/110 pre-treatment and maintain <185/105 throughout treatment.
- Labetalol OR Hydralazine OR Enalapril often used.
Acute Intracranial Hemorrhage
- Systolic BP >220 mmHg can be harmful.
- Debate exists over target BP, <140 mmHg or <180 mmHg systolic often used.
- Labetalol OR Esmolol OR Enalapril OR Phentolamine.
Sympathomimetics
- While not target organ damage, it may mimic other presentations (ACS, encephalopathy) and additional medications can be considered.
- IV Lorazepam for stimulants.
- Phentolamine OR Nitroglycerin OR Sodium Nitroprusside.
- Avoid beta-blockers (risk abrupt BP rise/coronary vasoconstriction due to catecholamines on unblocked alpha receptors).
Criteria For Hospital Admission
- Hypertensive Emergencies should be admitted to ICU for BP monitoring, intravenous antihypertensives, and target organ damage management.
Criteria For Safe Discharge Home
- A patient with a Hypertensive Emergency should not be discharged home.
- If no target organ damage, the patient does not require immediate treatment and can be discharged home (ie. Hypertensive Urgency/Severe Asymptomatic Hypertension).
- A patient with SBP >180 or DBP > 110 DBP can be diagnosed with hypertension according to Hypertension Canada guidelines.
- No immediate lowering of BP is necessary and rapid lowering of BP (IV meds) may cause harm due to the shifted autoregulation of BP; however,
- Canadian Emergency Medicine Cardiac Research and Education Group advises to consider oral antihypertensive therapy for these individuals >180 SBP or 110 DBP and to initiate treatment for SBP >230 or DBP >130.
- Follow-up should be arranged within 7 days and electrolytes checked within 1 week for ACE/ARB initiation.
Other Resources
- Figure 11 of AHA Guidelines.
- Table 19 of AHA Guidelines.
- Table 20 of AHA Guidelines.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
ICU admission: >1 high-quality, non-randomized trials or meta-analyses.
BP targets and specific antihypertensives: expert opinion/consensus.
Related Information
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Cardiovascular Emergencies
DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 20, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.