Foreign Body Ingestion – Diagnosis & Treatment
Ears, Eyes, Nose, and Throat, Gastrointestinal, Pediatrics
Context
- 75% of all Foreign Body Ingestions (FBIs) occur in children, typically between 6 months and 3 years of age.
- Often asymptomatic at time of presentation.
- Treatment guided by risk of complications: the type and size of object, time since ingestion, and location within the GI tract.
- Majority of foreign bodies pass spontaneously. 10-20% are removed endoscopically and <1% need surgical intervention.
Diagnostic Process
- Evaluation to ensure a patent airway should always be performed prior to proceeding.
History and Physical
- Type of object, time of ingestion, and the presence of any symptoms.
- Majority of patients are asymptomatic, but presenting signs and symptoms may include:
- Pain or discomfort in the throat, chest or abdomen
- Fever
- Coughing, wheeze or stridor
- Anorexia
- Dysphagia or gagging with oral intake
- Drooling
- Nausea
- Bloody stool, vomit, or saliva.
Laboratory Investigations
- Not required unless there is suspicion of severe complications (i.e. perforation).
Imaging
Endoscopy
- If signs and symptoms suggestive of esophageal obstruction, consider proceeding with emergent endoscopy without imaging.
Radiographs
- If not proceeding directly to endoscopy, evaluate with AP and lateral neck, chest, and abdominal radiographs for object identification and localization.
- All coin-shaped objects should be assumed to be button batteries until proven otherwise.
- Button batteries have a bilaminar structure, which appear as a double-ringed halo, and have a “step off” between the two flat ends.
CT
- Non-contrast CT considered if:
- FB identification and/or localization is not determined with plain x-ray and symptomatic.
- Complications suspected (i.e. perforation).
- The suspected FB considered dangerous (sharp, >2 cm wide, >5 cm long, or drug packets).
- May be used to evaluate for soft tissue injury.
Recommended Treatment
Indications for Emergent Endoscopic/Surgical Removal
- Airway compromise or difficulty with secretion clearance.
- High-grade esophageal obstruction.
- Button battery or sharp object located in the esophagus.
- Clinical presentation indicates complications.
Indications of Urgent Endoscopy
(within 24 hours)
- Blunt object not spontaneously progressing through the esophagus.
- Sharp, long (>5 cm), magnetic or super-absorptive objects prior to the proximal duodenum.
Indications of Non-Urgent Endoscopy
(within 24-72 hours)
- Large, blunt objects (>2-2.5 cm) proximal to the duodenum.
- Batteries in the stomach for >24-48 hours.
Expectant Management
- If patient is asymptomatic, and no indications for prompt removal, monitoring with serial radiographs on an outpatient basis is recommended.
- Patients should monitor themselves for any signs or symptoms of peritonitis, bowel perforation, or abdominal pain, and seek emergency care of present.
- Laxatives may be considered to expedite passage.
- See below for specific recommendations, grouped by specific object and location.
Management by Object Type and Location
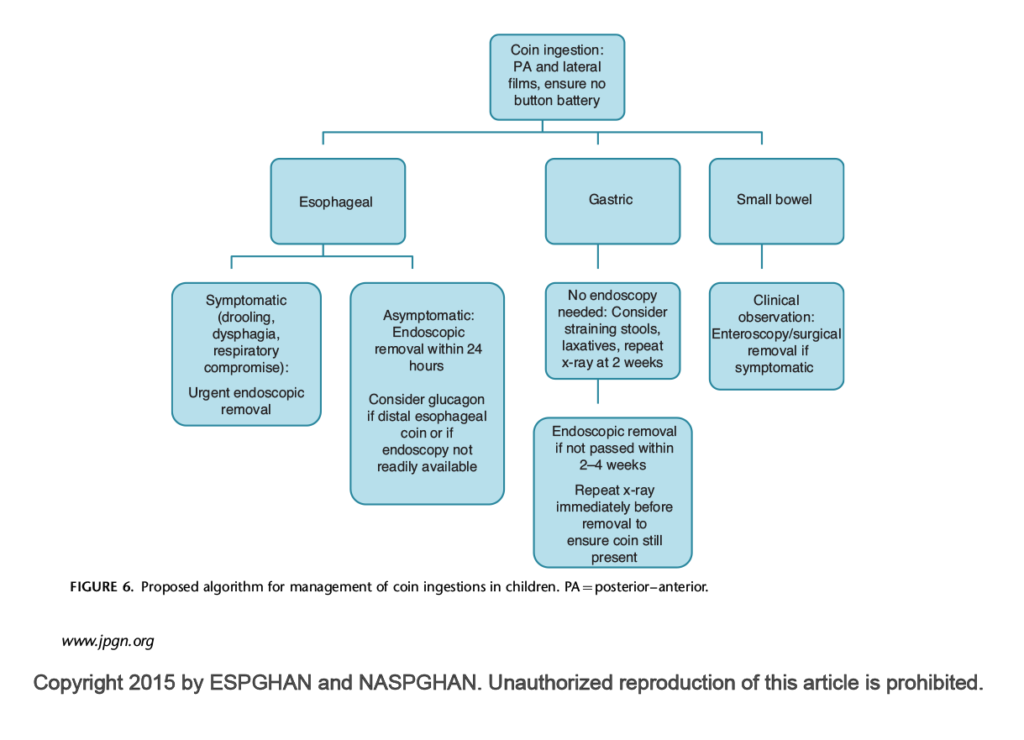
1. Coins, Blunt, or Long Objects
- General indications for urgent endoscopic or surgical removal:
- Patient symptomatic with object at any location.
- Blunt or spherical objects > 2-2.5 cm wide, or >6 cm long (>2.5cm in young children) proximal to the duodenum.
- Object in esophagus:
- Emergent removal if high-grade obstruction suspected.
- If asymptomatic, expectant management for up to 24 hours.
- Urgent removal indicated if patient symptomatic, if unknown time of ingestion, or if progression not observed via imaging by 24 hours after ingestion.
- Object in or distal to stomach:
- Outpatient expectant management to await spontaneous passage; removal indicated if object not passed by 3-4 weeks.
2. Batteries (typically button batteries)
- If suspected ingestion < 12 hours, and if not delaying endoscopic removal:
- 5-10 mL sucralfate (1g/10 mL) suspension PO every 10 minutes (up to 3 doses).
- Battery in esophagus:
- Emergent removal endoscopically (<2-6 hours) (i.e. GI, ENT, Gen Surg, etc.).
- Battery in or distal to stomach:
- Consideration prompt removal if: symptomatic, remains in stomach for > 48 hours, patient <5 years of age, or battery size >20 mm.
- Otherwise, outpatient expectant management for up to 2 weeks (examine stool; repeat x-rays).
- Other recommendations
- If evidence of esophageal injury, admit to hospital, place patient NPO (except for sucralfate indication above) & consider IV antibiotics.
- If low suspicion for perforation, irrigate esophageal injury with 50-150 mL of 0.25% sterile acetic acid post-removal – done by endoscopist.
- The use of emetics not recommended.
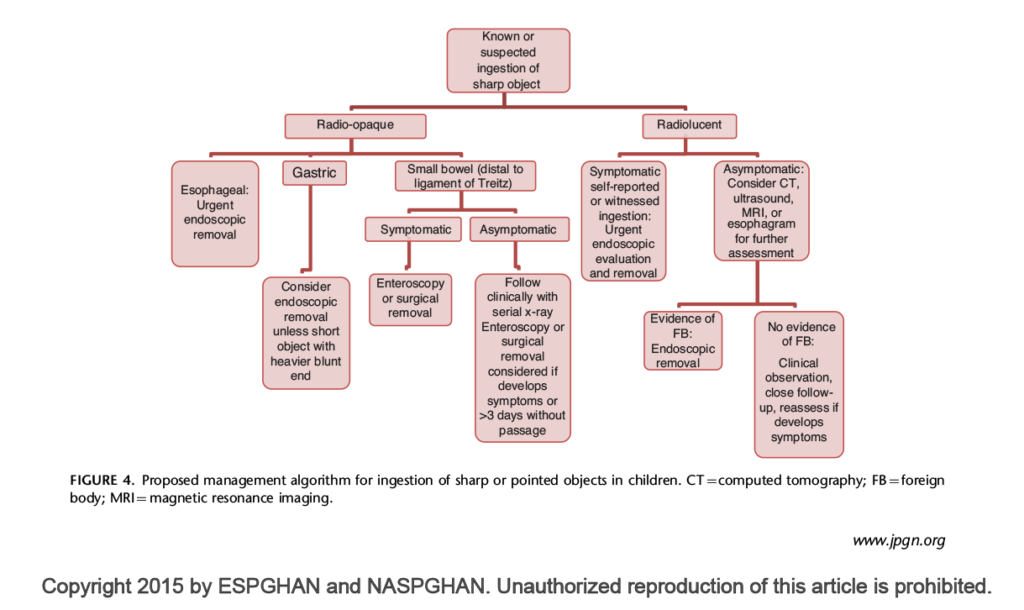
3. Sharp Objects (i.e. pins, needles, fish bones, etc.)
- Esophagus, stomach or proximal duodenum:
- Consult for immediate endoscopic removal.
- If signs of perforation or respiratory compromise, refer for immediate surgical consult.
- Distal to proximal duodenum:
- If signs and symptoms suggest bowel perforation or obstruction, or if no spontaneous progression for 3 days, refer for urgent surgical removal.
- If asymptomatic, outpatient expectant management to await spontaneous passage.
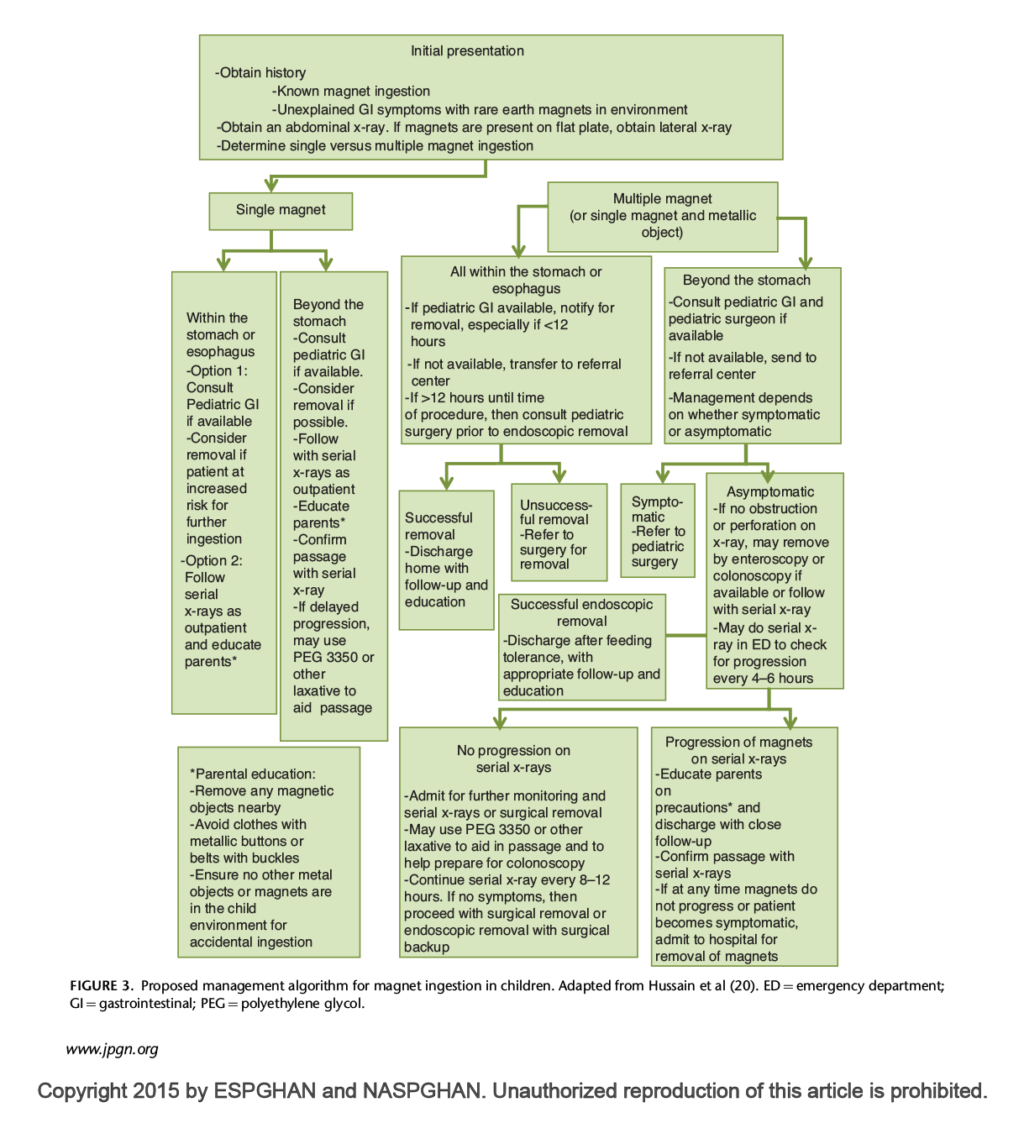
4. Magnets
- Single magnet
- Consult gastroenterology if pediatric.
- Outpatient expectant management is generally safe for asymptomatic patients at low risk for subsequent magnet ingestion.
- Removal should be strongly considered if object within endoscopic reach and performed if patient is symptomatic, or magnet not progressing spontaneously.
- Multiple magnets (or single magnet & second metallic FB).
- If child, consult with pediatric gastroenterology for endoscopic removal if < 12 hours since ingestion; or with pediatric surgery if > 12 hours.
- Immediate removal indicated if in esophagus or stomach or if patient is symptomatic.
- If asymptomatic and distal to stomach, serial radiographs every 4-6 hours in the ER.
- If spontaneous progression noted, discharge for expectant management.
- If no spontaneous progression noted, admit to hospital for continued monitoring and potential surgical removal.
- Other:
- Patient should be advised of magnet precautions.
- Avoid nearby magnetic objects.
- Avoid clothing with magnetic components (i.e. buttons, belts).
- Patient should be advised of magnet precautions.
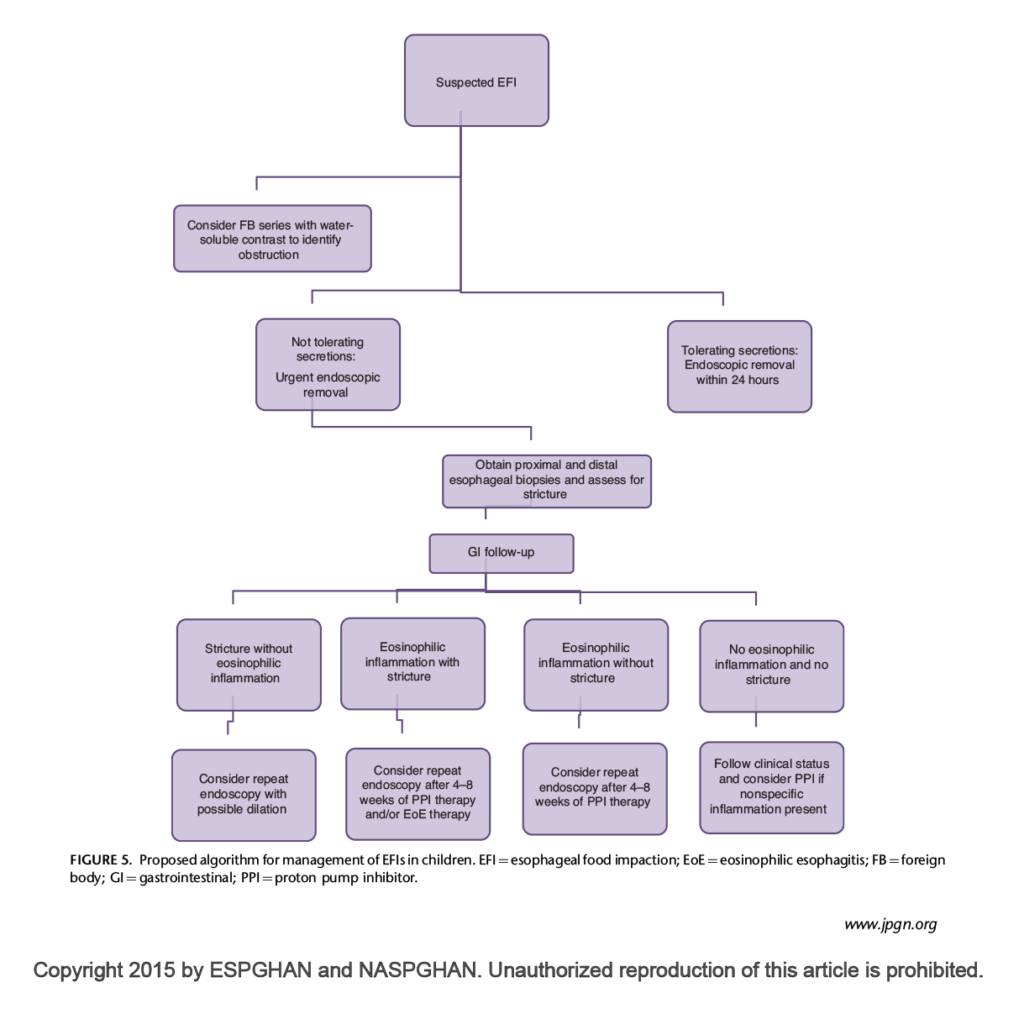
5. Esophageal Food Impaction
- Immediate removal indicated if patient in acute distress, or unable to swallow.
- If patient is stable and secretion clearance intact, observe for spontaneous progression for up to 24 hours before endoscopic removal.
- The use of glucagon (1 mg IV) may be considered in adults, though evidence is mixed
6. Superabsorbent Polymers
- The largest use of SAPs is found in personal disposable hygiene products, such as baby diapers, adult diapers and sanitary napkins.
- Emergent removal if within endoscopic reach.
- Requires monitoring for intestinal obstruction; objects may expand 30-60x in volume.
7. Lead Containing Objects
- Objects suspected to be high in lead content should be removed emergently.
- Administer acid-reducing agents (i.e. H2RAs, PPIs, antacids) to reduce acid-mediated dissolution.
- Monitor for symptoms of acute lead toxicity.
8. Caustic Liquids
- If ingestion unconfirmed, and asymptomatic, provide oral fluids as tolerated.
- Refer for endoscopy if deliberate consumption, or if signs of GI injury present.
- Avoid administering diluting or neutralizing agents prior to endoscopy.
9. Drug Packets
- Contact poison control centre or toxicology.
- Whole Bowel Irrigation with PEG 3350.
- If asymptomatic, observe with serial radiographs and monitor for signs of overdose; do not attempt removal, as this may cause packet rupture.
- Surgical intervention indicated if non-spontaneous progression, signs of obstruction, or suspected packet rupture.
10. Laundry Detergent Packs
- Caustic – dilute with milk/water.
- Endoscopy not recommended due to risk of aspiration.
Management
Magnet
Sharp Object
Esophageal Food Impaction
Coin Ingestion
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Guidelines are congruent amongst various national committees, and recommendations are rated as strong. It should be noted that the majority of recommendations are based on expert consensus and low-quality studies.
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 04, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.