Chest Wall Pain
Cardiovascular, Trauma
Context
- Chest wall pain accounts for up to a quarter of all patients in the ED who present with chest pain.
- Recommend an anatomic approach and classifying as traumatic or nontraumatic.
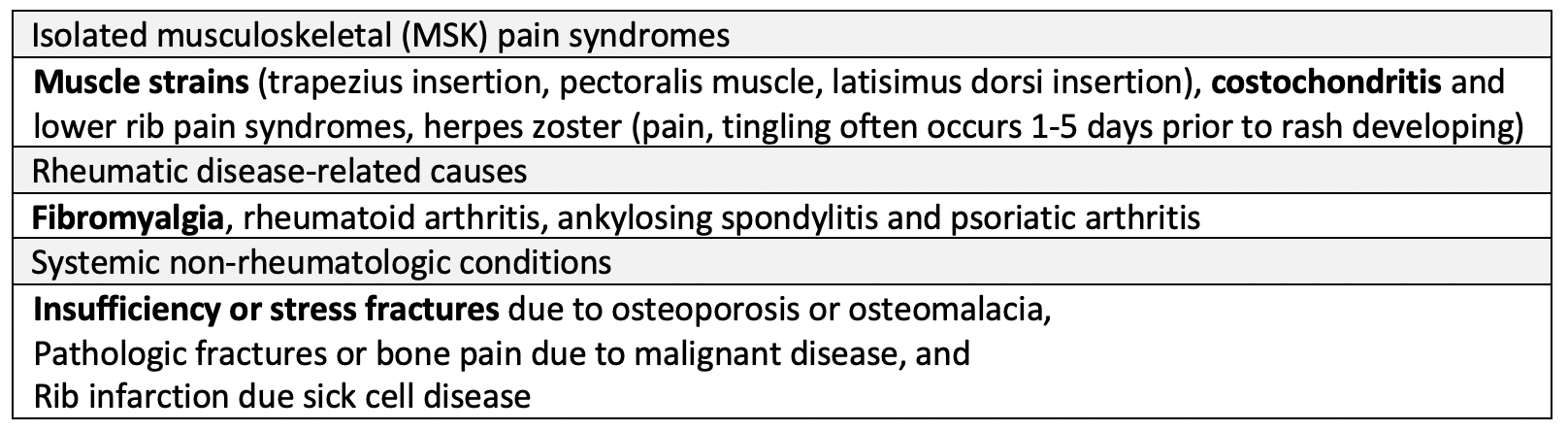
- Non-traumatic types of chest wall pain can be divided into the following 3 categories:
- Traumatic chest wall injury causing chest wall pain includes the following differential diagnosis:
- Osseous fracture(s), costochondral tear, nerve laceration, and soft tissue injuries (lacerations, muscle strains and contusions).
Diagnostic Process
Clinical findings associating with chest wall pain:
- At least 2 of the following: A. localized muscle tension; B. pain reproducible by palpation; C. stinging pain; D. absence of cough.
Differentiating features for non-traumatic chest wall pain in history:
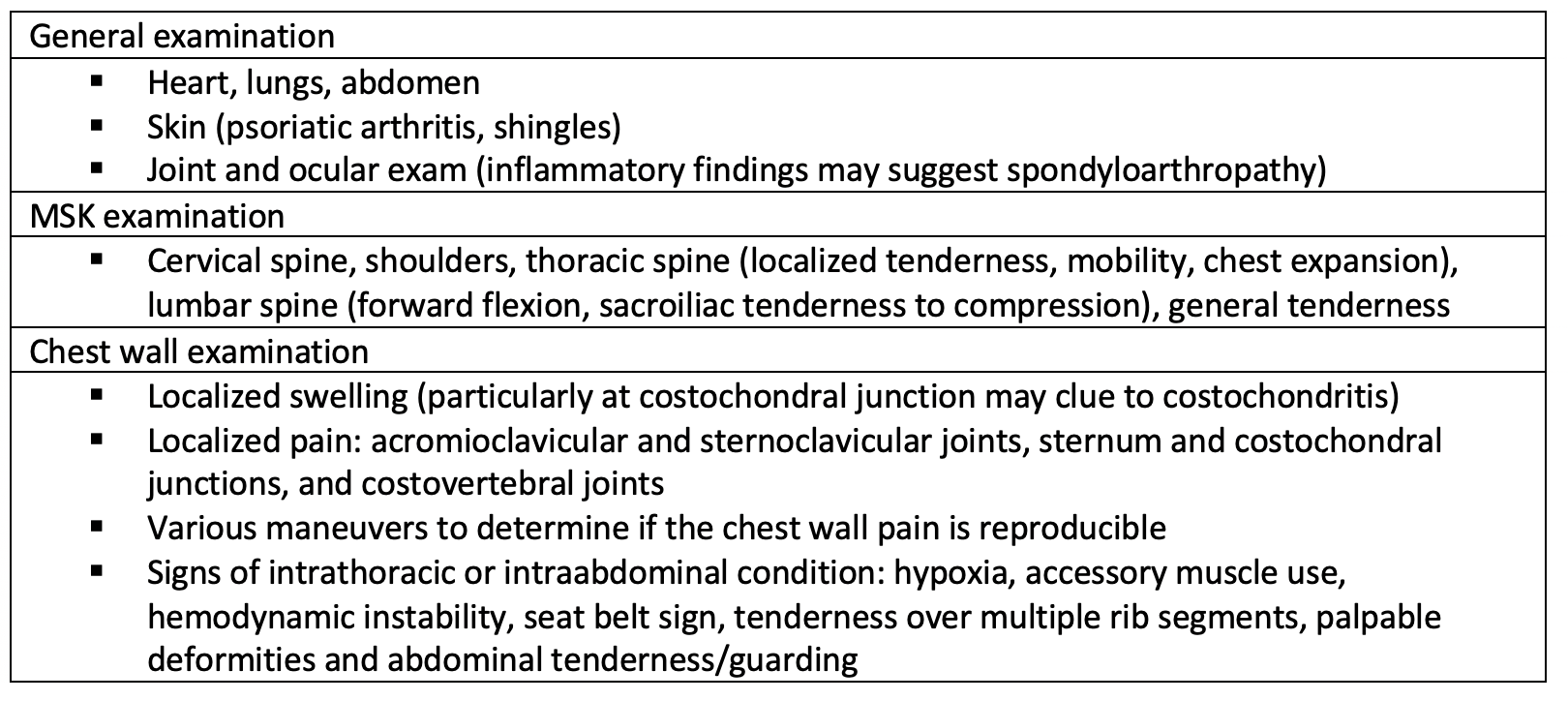
Physical examination for chest wall pain:
Investigations to consider:
- General: CBC, liver enzymes, renal function tests, urinalysis, chest radiography, ECG, other cardiac studies.
- Rheumatologic: ESR/CRP, rheumatoid factor, synovial fluid analysis and culture.
- Chest wall: rib, sternoclavicular and/or manubriosternal joint radiographs, CT imaging.
- Systemic non-rheumatologic disease: CT chest with or without IV contrast.
Clinical pitfalls:
- Chest wall pain does not exclude more serious and potentially life-threatening disorders:
- Ischemic heart disease
- Most common critical diagnosis not to miss.
- HEART Score.
- Classic symptoms and risk factors but can be atypical in elderly.
- Usually little to find on exam.
- ECG but may need serial troponins.
- Pulmonary embolism
- Risk factors – many have no known risk factor.
- Classic: sudden pleuritic CP and dyspnea.
- Syncope, persistent tachycardia.
- Use Wells and/or PERC Rules.
- D Dimer useful in low clinical suspicion.
- POCUS legs for DVT/cardiac for RV strain.
- Thoracic Aortic Dissection
- Risk factors = HTN; connective tissue disorder; late term pregnancy.
- Syncope.
- 1/3 have neurological deficits.
- Pulse deficit; new murmur of aortic regurgitation.
- CXR if low clinical suspicion.
- POCUS/CT.
- Boerhaave’s Syndrome
- Alcoholic (even without hx vomiting); recent scope/NG tube.
- CXR.
- Cardiac Tamponade
- Becks Triad – muffled hrt sounds, Elevated JVP, Hypotension.
- POCUS.
- Tension Pneumothorax
- POCUS.
- Incarcerated Diaphragmatic Hernia
- CXR, CT chest.
- ALSO consider:
- Cholecystitis
- Pericarditis
- Pyelonephritis
- Pneumonia
Other benign causes:
- Costochondritis (Tietze’s syndrome)
- Use caution when making this diagnosis – reserve it for classic presentations where there is clear marked tenderness over the costochondral joints.
- NSAIDs should improve pain and tenderness.
- ECG and CXR should be negative.
- GERD (Gastroesophageal reflux disease)
- Usually also have epigastric tenderness, provoked by food, alleviated by antacids.
- Esophageal spasm
- Clinical suspicion and response to Rx (Nitroglycerin) and negative cardiac WU if indicated.
- Psychogenic
- Anxiety and depression are very common in patients with chest pain.
- Try not to label pain as psychogenic in the ED setting,
- It is important to confirm that the patient is not experiencing chest pain due to any life threatening condition before proceeding to management of the chest wall tenderness.
Recommended Treatment
Approach to initial management:
- For trauma cases, evaluate for life threatening intrathoracic and intraabdominal injuries.
- abnormal vital signs, penetrating injury, altered mental status.
- Analgesics for pain relief
- Mild isolated chest wall pain (does not interfere with light activity)
- Acetaminophen (1st line) 1000 mg TID/QID maximum in adults.
- And/or an NSAID (naproxen over ibuprofen) in low to moderate dose:
- Ibuprofen 200-400 mg TID with food/glass of water.
- Naproxen 220-250 mg BID-TID with food/glass of water.
- Topical analgesics (capsaicin cream, salicylate-containing gel, diclofenac gel, lidocaine patch) may be added for a trial period up to 2 weeks to determine efficacy and discontinued if there is no benefit.
- Moderate chest wall pain (interferes with light to moderate activity)
- higher doses of naproxen or ibuprofen
- Ibuprofen 600-800 mg TID with food/glass of water.
- Naproxen 500 mg BID with food/glass of water.
- If a maximum acceptable dose of a particular NSAID has no benefit or becomes less effective, it is recommended to switch the class of NSAID.
- higher doses of naproxen or ibuprofen
- Severe chest wall pain (interferes with activities of daily living) – may need short course of narcotics. Avoid if possible.
- Gabapentin/pregapalin, cyclobenzaprine, and duloxetine may be tried if already taking above meds. Weak evidence for benefit. Should see effect in 2 weeks – reassessment with health care provider.
- Mild isolated chest wall pain (does not interfere with light activity)
Cautions:
- NSAIDs
- For patients at high risk of GI toxicity, alternative medication is vimovo or arthrotec, use of a selective COX-2 inhibitor (Celecoxib) or prophylactic PPI or misoprostol to prevent gastroduodenal damage.
-
Muscle relaxants are not recommended for older adult patients (age ≥ 65) with chest wall pain due to increased risk of adverse events.
Discharge notes:
- Patients with chest wall pain due to minor injuries or non-life threatening etiologies, and those at low risk of complications may be discharged following appropriate work-up and advised to return to the emergency department if there are new concerning symptoms (ex. shortness of breath, sudden increase in pain).
- A common patient concern is the assumption that their pain is due to heart disease, therefore, all patients should receive reassurance and education regarding their condition.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Chest wall pain is most often a diagnosis of exclusion. These recommendations are based on observational data and expert opinion.
Related Information
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Apr 26, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…



POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.