Alcohol Use Disorder (AUD)
Cardinal Presentations / Presenting Problems, Psychiatric and Behaviour, Substance Use, Toxicology
Context
- Alcohol Use Disorder (AUD) effects 10% of BC’s population and has a huge impact on acute care services, yet fewer than 1% of people with AUD ever receive medications shown to improve outcomes.
- AUD has a very high morbidity and mortality when untreated or under-treated.
- More than 35% of fentanyl overdoses in BC and 1/3 of all suicides involve alcohol. Over 7% of all Alcoholics die by suicide.
- The collateral damage to families and communities is huge.
- AUD is a very heterogeneous condition and this is one of the reasons pharmacotherapies have been under-prescribed.
- Initiating AUD pharmacotherapy whenever a patient presents with this disorder can dramatically improve their clinical course.
- Possible AUD medication side-effects or the need to trial a 2nd med, should not deflect us from trying to improve outcomes for people with AUD.
Recommended Treatment
- The goal can be to reduce intake and gradually detox over weeks, rather than precipitously. Pharmacotherapies can help with this transition.
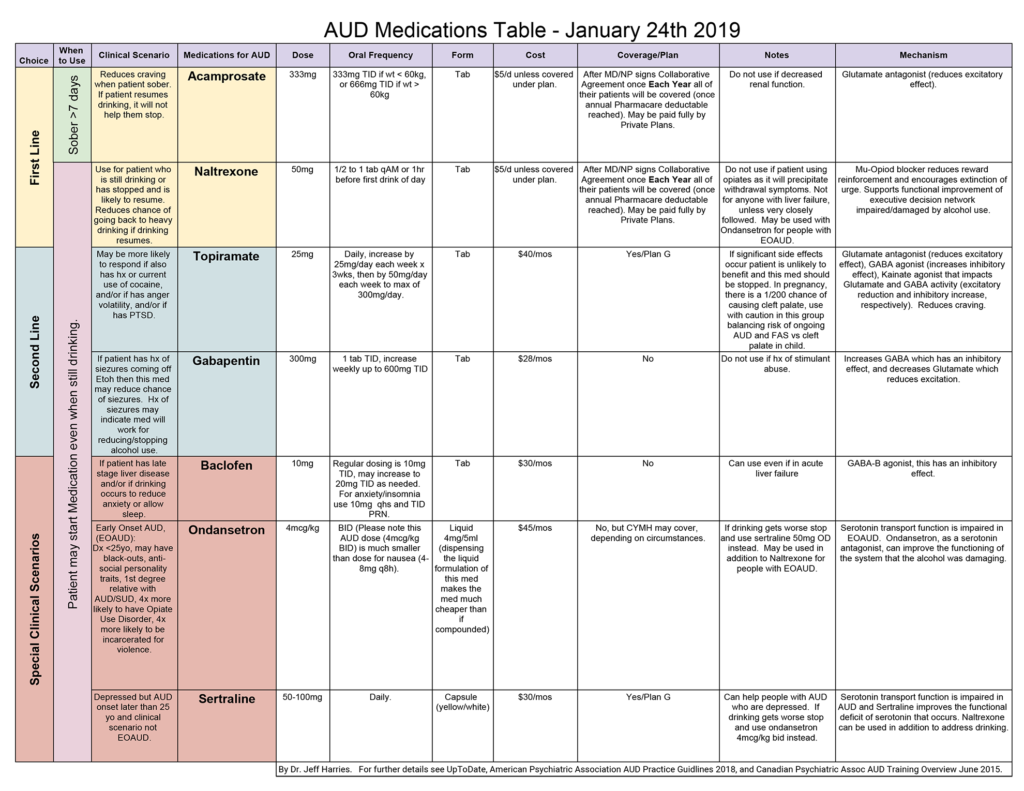
- Please see AUD Medication Table (below) for dosing recommendations.
- If a patient has a history of seizures, start patient on Gabapentin and Naltrexone.
- If patient has evidence of liver disease start on Baclofen +/- Naltrexone with close follow up of liver function to GP and/or clinic.
- If patient has history of significant cocaine or methamphetamine use, start patient on Topiramate.
- If patient has history of Early Onset AUD use Ondansetron and Naltrexone.
- If patient has been or will be sober for at least 7 days, start patient on Acamprosate.
- Antabuse is not recommended due to there being much better medication options in terms of effectiveness and safety.
AUD Medication Table (click to enlarge)
Criteria For Hospital Admission
- History of seizures recent or remote.
- Poly-substance abuse without support for AUD medication compliance.
- Acute alcohol withdrawal with high Clinical Institute Withdrawal Assessment (CIWA) high.
- Need for high dose of benzodiazepines.
Criteria For Close Observation And/or Consult
- Suicidal ideation in spite of new hope given with new plan of care that includes pharmacotherapy options.
Criteria For Safe Discharge Home
- Patient and/or family understands the plan of care ie. Take new meds and reduce, but don’t stop drinking (see NBC video)
- Follow-up with own MD or same walk-in clinic or see AUD Clinic if available.
- One page patient handout with resources on med supported AUD care.
- A referral service is available 24 hours a day to people across BC needing help with any kind of substance use issues. It provides information and referral to education, prevention, and treatment services and regulatory agencies.
The Alcohol & Drug Information and Referral Service
- Toll-Free: 1-800-663-1441
- Lower Mainland: 604-660-9382
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Related Information
OTHER RELEVANT INFORMATION
A Sober Approach: Can Modern Medicine Help Alcoholics Recover? (NBC; 12 minute Video)
Wasted… Nature of Things (CBC; 40 min Video)
American Psychiatric Association AUD Guidelines- January 2018
Exploring Treatment Options for Alcohol Use Disorders
– National Institute on Alcohol Abuse and AlcoholismThe Online Addiction Medicine Diploma – The BC Centre on Substance Use (BCCSU)
Collaborative Prescribing Agreement NALTREXONE and ACAMPROSATE for the Treatment of Alcohol Dependence – March 2019
Acknowledgement
Dr. Harries passed away Nov 2021 from complications from ALS. His tremendous passion for medicine and support for patients was profound and lives on through all his contributions in the field, including through his legacy with the Canadian Alcohol Use Disorder Society.
For more on Dr. Harries: https://www.pentictonherald.ca/news/article_8f51a0d0-440d-11ec-b9ec-cbddef76d947.html
Relevant Resources
RELEVANT RESEARCH IN BC
System Response to Toxicologic EmergenciesRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 15, 2018
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.