1st Trimester Bleeding: Miscarriage – Diagnosis
Obstetrics and Gynecology
Context
- Early Pregnancy Loss (EPL): Intrauterine pregnancy (IUP) loss < 20 weeks Gestational Age (GA).
- 80% occur in first 12 weeks GA.
- 15-25% of all pregnancies.
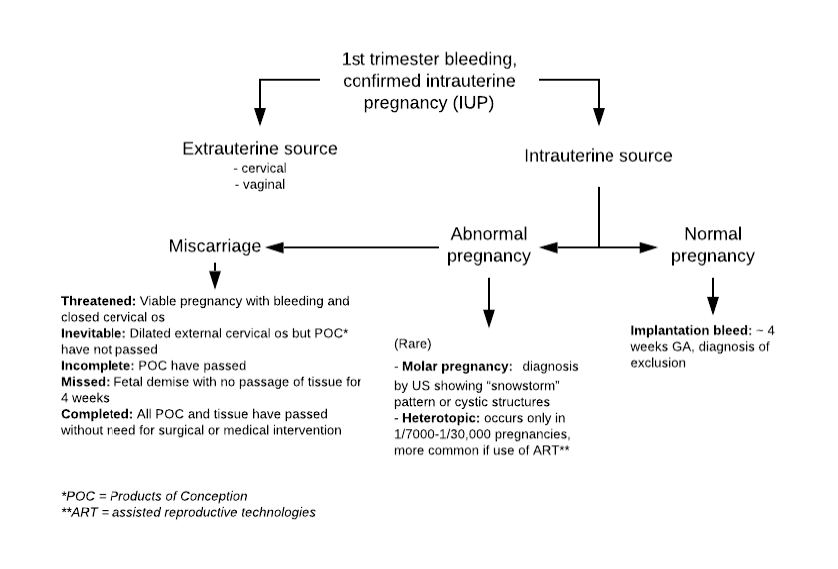
Differential Diagnosis for vaginal bleeding in context of IUP
Diagnostic Process
- Light bleeding or spotting in early pregnancy is common and does not increase risk of miscarriage.
- Pain and heavy bleeding (similar or greater than normal menses) increases risk of miscarriage (adjusted OR 2.84, 95% CI 1.93–4.56).
- With availability of US and β-hCG, pelvic exam is not required for diagnosis.
- Speculum exam if: high suspicion of extrauterine bleeding source, or to remove any clots or tissue from cervical os if severe bleeding, cramping, and hypotension.
- Quantitative β-hCG, CBC, Group and Screen (assess if Rhogam needed).
- Consider:
- Rhesus group – need Rhogam if Rh Negative:
- MICRhoGAM [Rho(D) Immune Globulin (Human)] (50 µg) (250 IU), prefilled syringe 50 micrograms IM.
- Urinalysis (UTI may trigger bleeding and/or EPL).
- Cross-match if bleeding severe or hemodynamically unstable.
- Rhesus group – need Rhogam if Rh Negative:
- All symptomatic patients with a positive pregnancy test should have a pelvic US, irrespective of β-hCG level.
- Initial assessment either with point-of-care ED ultrasound (POCUS) or diagnostic US by radiology.
- Gold standard is transvaginal US (TVUS) – in ED if provider proficient in US use, otherwise by radiology.
- Assess if IUP:
- US indeterminate or uterus empty rule out ectopic pregnancy (see PECS – pregnancy of unknown location, PUL).
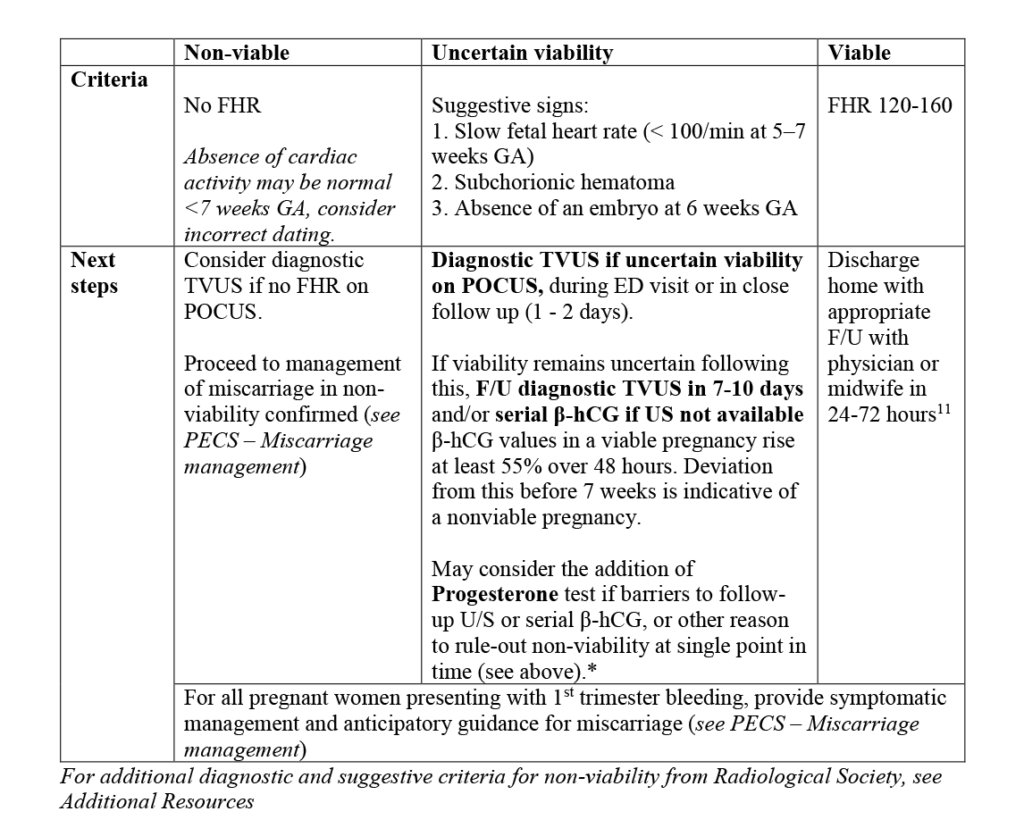
- Viable pregnancy?
* Serum progesterone: Consider if IUP of uncertain viability on U/S. Progesterone < 15 nmol/L has a sensitivity of 75% and specificity of 98% in predicting nonviable pregnancy. An elevated serum progesterone is therefore reassuring for viability. This test may be beneficial if there is a need to determine viability at a single point in time. If a follow up U/S and/or β-hCG is possible, then the addition of a serum Progesterone does not change management in the ED.
Follow up assessments with:
- With main OB provider.
- Early Pregnancy Assessment Clinic (EPAC).
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Progesterone as a test to assess pregnancy viability. There is a theoretical benefit according to a meta-analysis by Verhaegen et al. (2010), however the benefit of this test has not yet been assessed in an ED context.
- Obtain pelvic US on all pregnant patients irrespective of β-hCG.
- Reliability of POCUS in ED to identify IUP, cardiac activity.
- Deferral of pelvic exam when assessing threatened miscarriage.
Relevant Clinical Resources
- EM Rounds Blog (St John’s Hospital) on early pregnancy and PUL.
- Emergency Medicine Cases blog and podcast on early pregnancy complications.
- Breaking Bad News.
- Communicating with Families Experiencing Pregnancy Loss.
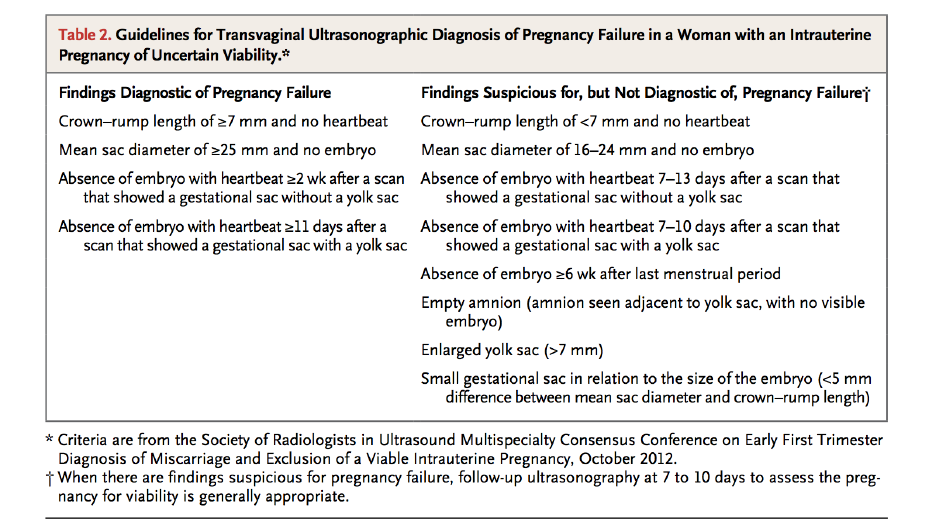
- Criteria are from the Society of Radiologists in Ultrasound Multispecialty Consensus Conference on Early First Trimester Diagnosis of Miscarriage and Exclusion of a Viable Intrauterine Pregnancy, October 2012:
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jul 23, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.