A troubling increase in the number of people declining transport to hospital after opioid overdoses.
British Columbia is still grappling with an opioid overdose epidemic – it is difficult to swallow given that the public health emergency was declared four years ago in 2016.
However, challenges often create the impetus for leadership, and proudly our emergency medicine community has stepped up. A recent CJEM article highlights the incredible work of local EM leaders. Dr. Andrew Kestler at St. Paul’s Hospital, Dr. Jason Wale in Victoria, and Dr. Melissa Allan in Burnaby are physician champions and pioneers for ED buprenorphine/naloxone programs in our province.
At Vancouver General Hospital, we are piloting the provision of take-home buprenorphine/naloxone packages at standard dosing and microdosing regimens. The VGH team is rolling out a multi-site evaluation of these dosing approaches. Together, the BC EM community is paving a path, and generating evidence, that will improve care for ED patients with opioid use disorder across Canada and beyond.
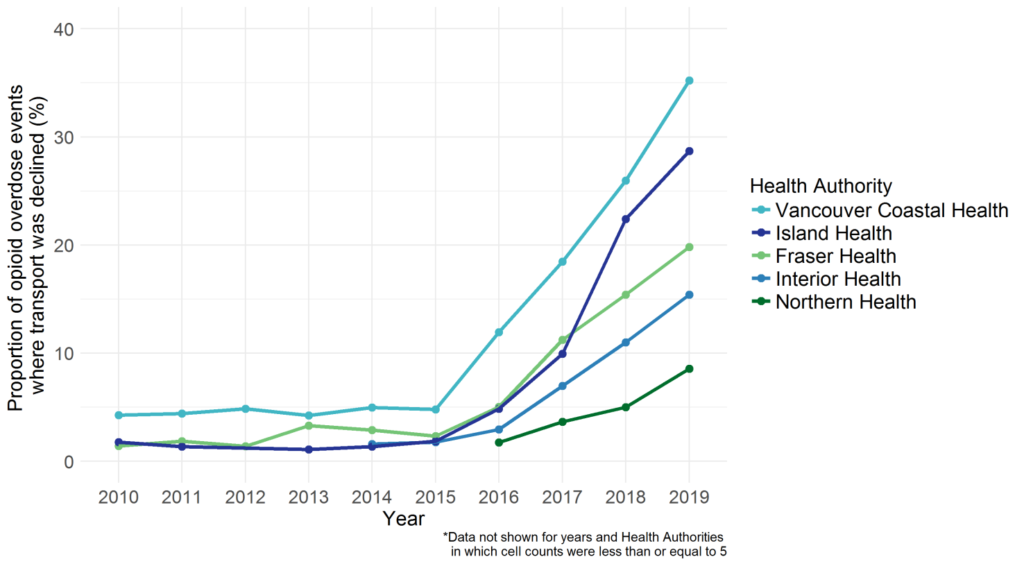
As the nuances of this evolving epidemic come to light, it is clear that emergency health services and emergency departments are critical points of contact for the population at risk of an opioid overdose. The BC Centre for Disease Control (BCCDC) has been receiving data from BC Emergency Health Services on paramedic-attended overdose events in BC since 2010. Recent analyses have revealed that calls to ambulances for opioid overdoses are on the rise, yet there has been a substantial increase in the number of people declining transport to hospital. Why we are seeing this trend remains unclear. Does it have to do with increased prevalence of take-home naloxone or more community services (like safe injection sites) where people are monitored outside of a hospital setting? Is it due to strained relations between people who use drugs and ambulance or emergency personnel? Is this a sign of general mistrust or encountered stigma among these patients with healthcare services in general?
We know that ambulance encounters and emergency department visits are fleeting opportunities to connect with and engage this difficult-to-reach and high-risk population, so this trend has important and troubling implications. We need to try to better understand why there is an increase in patients who have overdosed refusing ambulance transport to the hospital. We must try to understand the reasons from both the patient perspective and from you, frontline healthcare providers. Is this trend a surprise to you? Why do you think we are seeing this? Any and all opinions on this topic are welcome. Please comment below.
The BCCDC published a more detailed Knowledge Update from the Provincial Overdose Cohort on this topic – check it out!
Image 1. The proportion of paramedic-attended overdose events where transportation was declined, by Health Authority (2010-2019)
Disclaimer: The views and opinions expressed in this blog post are those of the authors and do not necessarily reflect the official policy or position of the BC Emergency Medicine Network.
COMMENTS (1)
Hi Jessica, Where did you obtain this data?
Add public comment…


Hi Jessica,
Where did you obtain this data?