Urinary Tract Infection (Adult) – Diagnosis
Cardinal Presentations / Presenting Problems, Infections, Urological
Context
- Common ED presentation.
- 10X more frequent in women.
- 1 in 5 women will have UTI in lifetime.
- Usually uncomplicated, treated with oral antibiotics.
Deifintions, Classification, Etiology
Definitions:
- Pyuria: WBC in urine.
- Bacteriuria: Bacteria in the urine, >10^5 colony forming units (CFU)/mL with culture.
Classification:
- Uncomplicated UTI/Cystitis:
- Lower tract infection
- Bladder (cystitis) and urethra (urethritis)
- Usually healthy non-pregnant women with no anatomical abnormalities
- Lower tract infection
- Complicated UTI:
- Upper tract infection
- Renal Parenchyma + collecting system (pyelonephritis)
- *Considered complicated if [3]:
- Male
- Pregnancy
- Urolithiasis
- Structural Abnormalities
- Catheters/Stents
- Antibiotic Failure
- Hospital-associated UTI
- Immunocompromised
- Malignancy
- Upper tract infection
Etiology:
- Urine should be sterile from glomerulus to external sphincter in male and bladder neck in females.
- Sterility is due to forward flow, urine acidity, immune system, mucosal barrier.
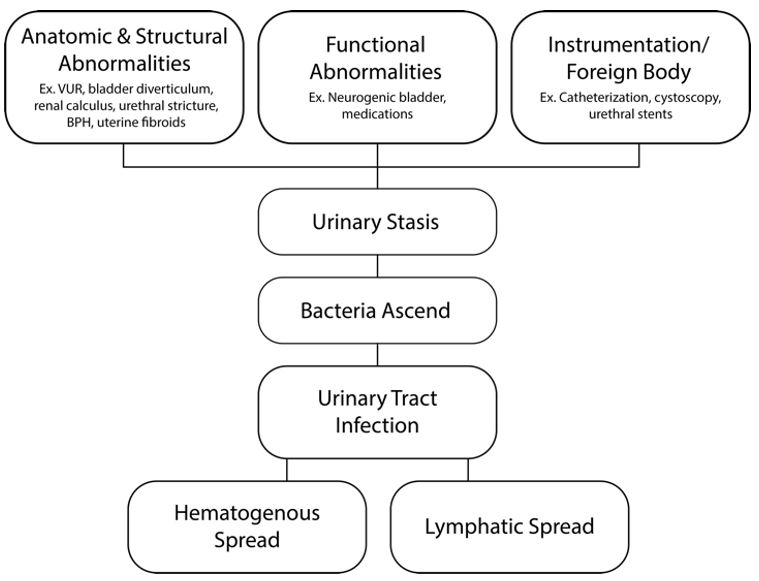
- Infections are caused by problems in anatomy, structure and function. Also instrumentation.
- Anatomy:
- Incompetence in ureterovesical valve –> vesicoureteral reflux (VUR)
- 1/3 children under 24 months with febrile UTI
- Neurogenic bladder
- Urologic Surgery
- Congenital urethral valves
- Bladder diverticulum
- Incompetence in ureterovesical valve –> vesicoureteral reflux (VUR)
- Structure:
- Calculi
- Intrinsic or extrinsic mass effect
- Example: Men – BPH, urethral stricture
- Example: Women – Fibroids, pregnant, uterine prolapse or cystocele
- Function:
- Dysfunction in bladder emptying
- Neurogenic bladder
- Drugs
- Anticholinergics
- Antihistamines
- Antipsychotics
- Antidepressants
- Antiparkinsonian
- Sympathomimetics
- Muscle Relaxants
- Instrumentation:
- Most common cause of nosocomial UTI is Foley catheters
- Lifestyle:
- Sexual intercourse, toilet hygiene
- Introduces bacteria into a woman’s urinary tract
- Evidence for cranberry as a UTI prophylactic
- Introduces bacteria into a woman’s urinary tract
- Sexual intercourse, toilet hygiene
- Dysfunction in bladder emptying
- Anatomy:
Created By Ella Barrett-Chan, MSI UBC
Microorganisms:
- Uncomplicated/Complicated: E.Coli (greater than 80%), Staphyloccus Saprophyticus (15%). Can include other gram negatives (Klebsiella, Proteus) and gram positive (enterococcus, GBS).
- Considerations:
- Complicated UTI (eg. catheter associated or elderly men) can be polymicrobial.
- Pseudomonas, Enterococcus faecium, ESBL result in complicated infections.
- Fluoroquinolone resistance increasing.
Diagnostic Process
- Stable vs Unstable Patient
- UTI vs UTI Mimic (see differential below)
- Simple vs Complicated UTI
History:
- Cystitis: Can include dysuria, urinary frequency, urgency, hematuria
- Pyelonephritis: Can include progression of cystitis to fever, nausea/vomiting, flank pain
- *Include questions to cover differential (see below). Examples:
- Abnormal vaginal discharge or bleeding? Dyspareunia?
- Unprotected sexual intercourse?
- Last Menstrual Period
- Note: Atypical presentations are not uncommon in the elderly
Physical Exam:
- Suprapubic tenderness on abdominal exam
- CVA tenderness common in pyelonephritis
- Vital sign abnormalities in complicated UTI (eg. sepsis)
- *Include exam to cover a differential. Examples:
- Vaginal/Cervical exam
- Testicular Exam
- Abdominal Ultrasound to assess for Abdominal Aortic Aneurysm [see video]
*Differential Diagnosis (UTI mimics) [3]:
- Bacterial Vaginosis
- Sexually transmitted disease (STD)
- Pelvic inflammatory disease (PID)
- Epididymitis/orchitis
- Testicular/ovarian torsion
- Ectopic Pregnancy
- Cholecystitis
- Urolithiasis
- Renal abscess, infarction or thromboembolism
- Appendicitis
- Abdominal Aortic Aneurysm
Urine Dipstick:
- Most commonly used method to diagnose UTI
- Similar sensitivity and specificity to microscopy
- Leukocyte Esterase – marker of pyuria
- Diagnosis: Sensitivity 75 – 96%, Specificity 94-98%
- False Negative with antibiotic therapy, glycosuria, proteinuria
- Nitrite – marker of bacteria that convert nitrate to nitrite
- Diagnosis: Sensitivity 35-85%, Specificity 95%
- False Negative with non-nitrate-reducing bacteria (S. saprophyticus, Pseudomonas, enterococci)
- Leukocyte Esterase and Nitrite:
- Diagnosis: Sensitivity 75-90%, Specificity ~ 100%
- “What if clinically suggestive of UTI, but both Leukocyte Esterase and Nitrite negative?”
- May still require antibiotics as there are chances for false negatives.
- Self diagnosis has positive likelihood ratio of 4 (absence of vaginitis symptoms, likelihood ratio of 24)
- Clinical gestalt is important.
- “What if asymptomatic but positive leukocyte esterase and/or nitrite?”
- May not require antibiotics. Patient factors (eg. Pregnancy, Immunocomprimised) are important in decision making. See UTI Special Considerations section on Asymptomatic Bacteriuria for more details.
- Leukocyte Esterase – marker of pyuria
Microscopy:
- Optional but perform in recurrent UTI
- Can determine if sample contaminated
- > 10 WBC/mm^3 (non-centrifuged) or > 2-5 WBC/mm^3 (centrifuged) indicative of UTI
- >= 15 bacteria per high power field indicative of UTI
- WBC casts suggestive of Pyelonephritis
- Hematuria helpful in UTI diagnosis
- Note: UTI diagnosis can be made with microscopic bacteriuria and pyuria (+/- hematuria)
Urine culture:
- Not done in cases of uncomplicated UTI (clinical diagnosis)
- Perform in complicated UTI or recent antibiotic use
- Positive when:
- Suprapubic sample: any bacteria
- Urethral Catheter: >10^2 cfu/mL, single uropathogen, clinical symptoms
- Non-catheter: >10^5 cfu/mL
- >10^2 cfu/mL if known uropathogen in patient with clinical symptoms
Blood Cultures:
- Do not usually alter management
- Usually concordant with urine culture
- Perform in cases of sepsis or septic shock. Can consider in elderly, immunocompromised, urinary tract obstruction
Imaging:
- Not necessary in simple cystitis
- Use if concerned for mimics
- Consider for complicated UTI
- No role for plain radiographs
- KUB sensitivity 45-59 %/specificity ~77% (for renal pathology)
- Ultrasound
- Ideal in cases involving pelvic structures
- Can visualize hydronephrosis
- Sensitivity ~80%, Specificity 73%
- See video: renal ultrasound
- CT is frequently used in complicated UTI
- Most sensitive test for renal pathology
- If concerned about severe disease, or UTI mimics, CT is warranted
- IV contrast if concerned for embolus or thrombus
- Most sensitive test for renal pathology
Clinical scenario
STD vs UTI
- Can be difficult to distinguish because of overlap in symptoms (eg. dysuria)
- STD symptoms more gradual in onset and includes vaginal discharge/bleeding, pruritus, dyspareunia. Not typical to have change in urinary frequency/urgency.
- Assess for STD risk factors including a sexual history
- Perform vaginal/cervical exam and swabs
- Can consider treatment of both concurrently
- Tomas et al. performed an observational cohort study concluding the following:
- UTI’s are over diagnosed and STD’s are underdiagnosed in the emergency department
- STD’s can have abnormalities in urinalysis – positive leukocyte esterase or pyuria (defined as more than 5 WBC per HPF)
- Positive urinalysis does not equal UTI. Can have false positives (eg. STD, asymptomatic bacteruria)
- Recommendation:
- STD’s are a common UTI mimic. Take an appropriate history and physical exam/investigations. Consider treating both. Use clinical gestalt. Have appropriate follow-up.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The above summary is taken from recent literature reviews on emergency department diagnosis and management of UTI’s.
Related Information
Reference List
Related Information
OTHER RELEVANT INFORMATION
Relevant Resources
RELEVANT RESEARCH IN BC
Sepsis and Soft Tissue InfectionsRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 11, 2019
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.