Treatment of Persons with Inherited Bleeding Disorders (PwIBD) in the Emergency Room
Hematological / Oncological, Infections, Special Populations
First 5 Minutes
FACTOR FIRST CARD: Guidelines for Emergency Management of Hemophilia and Von Willebrand Disease
https://www.hemophilia.ca/wp-content/uploads/2022/06/FactorFirst-card-JUNE-2022.pdf
- PROMPT TRIAGE AND ASSESSMENT. PwIBD should be triaged urgently as delays in administering appropriate therapy, can significantly affect morbidity and mortality.
- DETERMINE THE LOCATION AND SEVERITY OF BLEED. Treatment for a suspected bleeding episode should be based on clinical history, findings could be normal in the early stages.
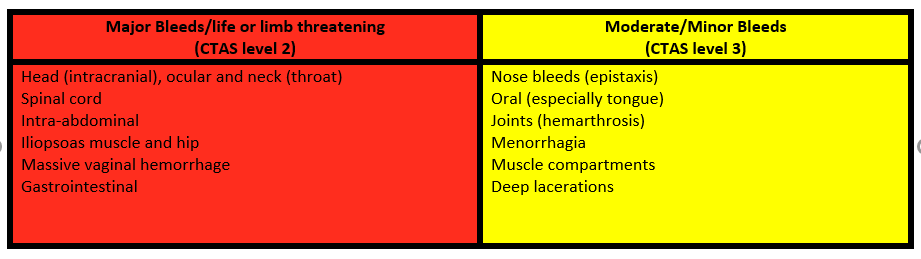
- POTENTIALLY LIFE THREATENING bleeds to the head, spine, abdomen or pelvis could initially be occult. An occult hemorrhage that progresses may produce emergent circumstances.
- ASK THE PATIENT if they have a Factor/Treat First Card or if they are followed by the Adult or Pediatric Bleeding Disorder Program of BC/Yukon. This treatment card provides patient specific dosing for major/minor bleeds and contact information for the programs.
- TREAT FIRST > INVESTIGATE LATER. It is recommended that treatment be given before any diagnostics studies (i.e., X-rays, CT scans, etc.) are performed to evaluate a suspected bleeding problem or injury, especially in the case of head trauma or suspected intracranial hemorrhage. Early treatment can mitigate further bleeding or complications.
Context
Inherited Bleeding Disorders are rare and when an affected person accesses the ER, historically healthcare providers have not always recognized the urgency of providing timely hemostatic interventions and connecting with experts who can help.
- PwIBD do not bleed more at the time of injury/procedure they do however, bleed for a longer duration causing increased risk of infection, poor healing/recovery, anxiety, hospital admissions and disabilities.
- The BC Bleeding Disorder Programs of BC/Yukon support these patients over the course of their lives.
- PwIBD include: von Willebrand Disease (Types 1, 2A, 2B, 2N, 2M, 3), Factor VIII (8) Deficiency (Hemophilia A), Factor IX (9) Deficiency (Hemophilia B/Christmas Disease), Factor XI (11) Deficiency (Hemophilia C), platelet disorders, other rare factor deficiencies (i.e., fibrinogen, FII, FV, FVII, FX, FXIII) and Undefined Bleeding Disorders (UBD). UBD is defined as a person with a clear bleeding tendency (positive bleeding score) in the presence of normal haemostatic tests.
- Normal Factor VIII (8), Factor IX (9), vWF:Ricof Levels: 0.50-1.5 U or 50-150 %
- Factor VIII (8) & IX (9) classifications: Severe <1 %; Moderate 1-5 %; Mild 5- <40%
- When bleeding disorders are classified as “Mild”, it does not suggest that poor outcomes or death will NOT occur without treatment. All too often healthcare providers are unduly influenced by the term mild.
- This population Infrequently bleeds and are often unsure when to seek help.
- They have Limited experience with signs & symptoms of bleeding and may present late to ER.
- Often Do not self-infuse and need to access a hospital setting or clinic for treatment.
Diagnostic Process
- TREAT FIRST > INVESTIGATE LATER. For a PwIBD it is recommended that treatment should be given before any diagnostics studies (i.e., X-rays, CT scans, etc.) are performed.
- AVOID UNNEEDED PROCEDURES however, for a PwIBD who has an illness that requires an invasive procedure ensure the patient has had appropriate factor/hemostatic treatment before starting the procedure. Also, consider traumatic repeated venipunctures may cause painful hematomas and limit further IV access.
- AVOID UNNEEDED FACTOR LEVELS. For PwIBD followed by a BC Bleeding Disorder Program, there is no need to order factor levels during the initial admission as the clinical severity of a patient’s bleeding disorder is gauged by their baseline clotting factor level, a value that remains fairly constant throughout that person’s life.
- SCREENING ASSAYS (i.e., aPTT, one stage factor levels) in some cases will NOT be accurate/reliable depending on the prophylaxis product (i.e., Emicizumab, Rebinyn) the PwIBD is using.
- AVOID INTRAMUSCULAR INJECTIONS including immunizations, if possible. If they must be given, treatment may be required preceding the injection.
If the patient has NEVER been seen by a hematologist or one of the BC programs, a hematology consult should be completed promptly and the patient referred to the age appropriate program.
Consider completing a bleeding history, The International Society on Thrombosis and Hemostasis Bleeding Assessment Tool may be used to guide questioning.
- Adult Bleeding Disorder Program of BC/Yukon referral form: https://hemophilia.providencehealthcare.org/programs-services/referrals
- Pediatric Bleeding Disorder Program of BC/Yukon referral form: http://www.bcchildrens.ca/health-professionals/refer-a-patient/hematology-referral
Recommended Treatment
Emergency care of PwIBD sustaining an injury/bleed should include consideration that there could be insidious bleeding.
SOURCES for treatment recommendations:
- THE PATIENT, ask what treatments they typically receive. If the patient self-infuses independently at home ask if they have already infused (time, type of factor, dose). Patients often are very knowledgeable about their bleeding disorder.
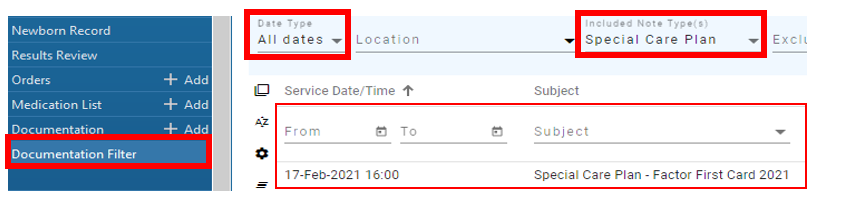
- FACTOR/TREAT FIRST CARD, if the patient does not have their card with them, search for a recent “Hematology note” on BC Care Connect, which should contain recommendations for major/minor bleed treatments.
- SPECIAL CARE PLAN, in VCHA Cerner look for the Special Care Plan-Factor First Card. To access the document: click “documentation filter” menu (left side), search note type(s) “Special Care Plan”, ensure date type is “all dates”.
- CALL THE AGE APPROPRIATE BLEEDING DISORDER PROGRAM for recommendations if the patient is followed by one of the clinics.
- Adult Bleeding Disorder Program of BC/Yukon
P:604.806.8855 ext 1 F:604.806.8784 Email: H&Hclinics@providencehealth.bc.ca
P:604.682.2344 After hours, w/e and stats call hematology on call at St Paul’s Hospital.
https://www.providencehealthcare.org/hemophilia-program - Pediatric Bleeding Disorder Program of BC/Yukon
P:604.875.2406 F:604.875.2911 Email: hemophilia_clinic@cw.bc.ca
P:604.875.2161 After hours, w/e and stats call hematology on call at BC Children’s Hospital (BCCH)
http://www.bcchildrens.ca/our-services/clinics/cancer-blood-disorders/inherited-bleeding-disorders
- Adult Bleeding Disorder Program of BC/Yukon
- FACTOR PRODUCTS are ordered from the hospital Transfusion Medicine Laboratory NOT pharmacy.
- BLOOD CONSENT is required only for plasma derived factor concentrates (i.e., Humate P, FEIBA).
- ASA/NSAIDs are relatively contraindicated in PwIBD population due to bleeding.
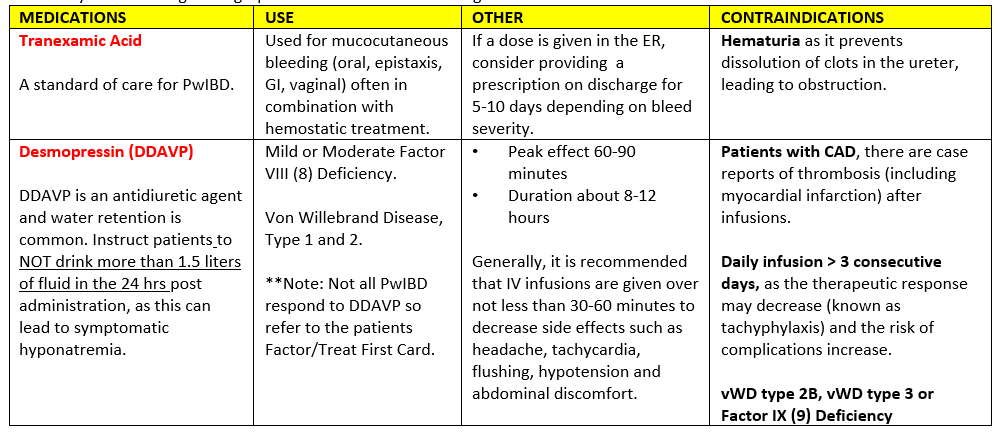
- Refer to your local drug monographs and consider the following:
Criteria For Hospital Admission
- Sustained a MAJOR INJURY/BLEED or at risk for compartment syndrome, consider for admission/observation and reimaging.
- Patient is UNABLE TO SELF INFUSE factor products and requires ongoing treatment.
- UNCLEAR PATIENT ABILITY to observe for complications or difficulty establishing a follow-up plan.
Criteria For Transfer To Another Facility
- If major injury/bleed, patient may require transfer to a facility with ICU and 24/7 inpatient hematology support with a coagulation laboratory. For adult patients consider transfer to St Paul’s Hospital or Vancouver General Hospital, for pediatric patients transfer to BC Children’s Hospital (BCCH).
- If a PwIBD requires transportation to another facility for definitive care, all efforts should be made to provide appropriate hemostatic treatment before transport.
Criteria For Close Observation And/or Consult
- Close observation is required if the patient has sustained a major injury/bleed, or at risk for compartment syndrome, and reimaging should be considered.
- If followed by a bleeding disorder program consult the age appropriate program.
- For a new diagnosis consult hematology and refer on to the age appropriate program.
Criteria For Safe Discharge Home
- Reliable and informed patient with means to return if needed.
- Provide clear discharge instructions and discuss a follow-up plan.
- Ensure they have appropriate prescriptions on discharge.
- If followed by a BC Bleeding Disorder Program send an ER discharge summary to the age appropriate program (i.e., ‘SPH Adult Bleeding Disorder Clinic” in VCHA/VIHA Cerner).
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
WFH Guidelines for the Management of Hemophilia and Guidelines on the Diagnosis of von Willebrand Disease, serve as a resource to support education, advocacy, and decision-making related to bleeding disorders treatment and the delivery of care around the world, including developed and underdeveloped countries.
Related Information
OTHER RELEVANT INFORMATION
If followed by a bleeding disorder program request the patient follows up with the program on discharge.
If this is a new diagnosis ensure the age appropriate program referral has been completed & sent, ensure to provide the patient with the clinic contact information.
A guide to help self administer DDAVP in the context of a bleeding disorder: https://precare.ca/ddavp/
Reference List
Srivastava A, Santagostino E, Dougall A, et al. WFH Guidelines for the Management of Hemophilia, 3rd ed. Haemophilia. 2020;26(Suppl 6): 1-158. Available from https://onlinelibrary.wiley.com/doi/10.1111/hae.14046
James P, Connell N, Ameer B, et al. ASH ISTH NHF WFH 2021 guidelines on the diagnosis of von Willebrand Disease. Blood Advances. 2021;5 (1): 280-300. Available from https://doi.org/10.1182/bloodadvances.2020003265
Bullard MJ, Chan T, Brayman C, et al. Members of the CTAS National Working Group. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) Guidelines. CJEM. 2014 Nov.16(6):485-9. PMID: 25358280.
Canadian Hemophilia Society. Emergency Care. Canadian Hemophilia Society. Accessed May 19 2023. https://www.hemophilia.ca/emergency
Rodeghiero F, Tosetto A, Abshire T, et al. ISTH/SSC joint VWF and Perinatal/Pediatric Hemostasis Subcommittees Working Group. ISTH/SSC bleeding assessment tool: a standardized questionnaire and a proposal for a new bleeding score for inherited bleeding disorders. J Thromb Haemost. 2010 Sep;8(9):2063-5. doi: 10.1111/j.1538-7836.2010.03975.x. PMID: 20626619. ISTH-SSC Bleeding Assessment Tool for healthcare providers: Available from https://bleedingscore.certe.nl/
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Apr 10, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.