Toxic Shock Syndrome – Diagnosis
Infections, Toxicology
Context
- Toxic Shock Syndrome (TSS) is a severe systemic illness characterized by a constellation of symptoms: shock, fever, erythematous or desquamating rash, GI symptoms, and CNS disturbances. It is often mistaken for viral illness or septic shock.
- It is caused by some subgroups of Staph or Strep which produce exotoxins (ex. staphylococcal TSST-1) that act as a superantigen, over-activating the immune system by bypassing the usual steps of the immune sequence.
- Staphylococcal TSS:
- less common.
- younger, healthier patients – pediatric patients are much less likely to have anti-TSST-1 antibodies.
- typical source is mucosal colonization with clinically silent or unimpressive infection; classically a tampon, nasal packing, or postpartum.
- burns and burn dressings, especially in pediatric patients with a low TBSA burn, are a more common source since the decline of synthetic high-absorbency menstrual products.
- Streptococcal TSS:
- more common, and increasing prevalence.
- higher mortality.
- occurs as a result of invasive streptococcal infection – often a skin or soft tissue infection (like Necrotizing Fasciitis) which is less likely to be occult.
- If unidentified and untreated, TSS can have a high mortality (up to 50%!)
- Staphylococcal TSS:
Presenting
- Flu-like Prodrome:
- Fever, chills, headache, myalgias.
- GI symptoms, sometimes a sore throat.
- Often misdiagnosed as viral illness; at this stage, usually does not appear “toxic.”
- Skin findings:
- Classically, diffuse erythematous rash, but may have essentially any rash finding.
- Mucosal erythema is common.
- Desquamation is classic, but is a delayed finding – not expected until weeks later.
- Multisystem Organ Failure
- Tachycardia, myocardial dysfunction, hypotension.
- Renal failure – often the first sign of organ injury, typically preceding hypotension, and at an earlier stage and greater severity than expected for a similar degree of septic shock.
- Delirium – irritability or vague confusion is classic, without any overt agitation or focal neurologic features.
- WBC may also be normal, but commonly with a high Neutrophil:Lymphocytes ratio. Early Lymphopenia has been proposed as a specific factor to aid in this diagnosis.
- Hyponatremia has also been proposed as a more specific factor, especially in combination with Lymphopenia.
- Elevated CK, AST, ALT and Bili.
- Thrombocytopenia is typically late, and an ominous finding.
- For Staphylococcal TSS, blood cultures are almost always negative. They are useful to exclude alternate diagnoses, but not helpful in the acute diagnostic phase.
- For Streptococcal TSS, blood cultures are commonly, but not universally, positive.
Diagnostic Process
- The commonly referenced CDC diagnostic criteria were designed for epidemiologic research, to define retrospectively with a high degree of specificity whether patients fit the typical description of Toxic Shock Syndrome along the entire course of their illness:
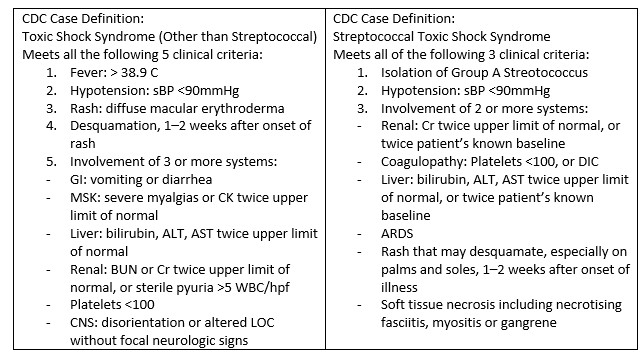
- These case definitions were not designed for everyday clinical practice or for safe, early recognition.
- Some required components are not expected early in the clinical course, and some do not appear until weeks later (for example, desquamation).
- A patient does not need to fully meet these criteria for treatment to be indicated and life-saving.
Abbreviated Criteria:
- Fever > 39
- Rash
- Diarrhea +/- Vomiting
- Irritability
- Lymphopenia
- In the ED, our priority should be early consideration, with a presumptive diagnosis made based on a clinical gestalt of how well the patient fits these typical features, and the likelihood of alternate diagnoses.
- Avoiding irreversible organ failure depends upon early initiation of treatment, before the patient meets the CDC Case Definition. Treatment is comparatively benign and can later be withdrawn if an alternate diagnosis is made.
- The ultimate diagnosis of TSS may be retrospectively applied according to the CDC case definition later in the clinical course, although early treatment may halt the pathological process resulting in “Aborted TSS.”
Recommended Treatment
- Contact + Droplet Precautions
- Some strains of Streptococcus are more toxogenic than others and outbreaks have been reported.
- High Quality Supportive Care
- High dependency care space – HAU or ICU often required.
- IV fluid resuscitation, targeting euvolemia and normal urine output.
- Vasopressors or Inotropes if required.
- No robust evidence to direct vasopressor selection; Norepinephrine likely still the best first choice.
- Patients with TSS seem to exhibit early myocardial dysfunction, possibly from direct myocardial effects of the toxins, or from robust cytokine release. Consider earlier addition of inotropes compared to the usual septic shock algorithm.
- Steroids if refractory shock, as per septic shock algorithms.
- Beta Lactam Antibiotics to treat both Staphylococcus and Streptococcus, even if infectious source appears benign or subtle.
- Toxin-Suppressive Antibiotics:
- Clindamycin 900mg IV which inhibits protein synthesis in 99% of Group A Strep and some Staphylococcus.
- This prevents toxin generation by the infectious bacteria until they can be eliminated by antibiotics or source control.
- It does not eliminate or neutralize toxin that has already been released; this will be cleared over several days.
- Clindamycin 900mg IV which inhibits protein synthesis in 99% of Group A Strep and some Staphylococcus.
Related Information
OTHER RELEVANT INFORMATION
Source
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Mar 31, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.