Syncope
Cardiovascular
Context
- Syncope is a sudden transient loss of consciousness (LOC) with spontaneous complete recovery. Near syncope is considered equivalent to syncope.
- 7-day risk of serious adverse outcome is 10% and death is 1/2501.
- Despite several risk stratification rules (below), the best diagnostic tools remain: careful history, thorough physical exam, and ECG and good clinical judgement.
Pathophysiology, history, and physical exam
Cardiac
Mortality >10% at 6 months.
- Arrhythmias: Most common cause of cardiac syncope.
- No prodrome.
- Sudden LOC and may report palpitations prior to the event.
- Occurs in any position.
- Family history of arrhythmia, inherited cardiac disorders, sudden unexplained cardiac death, drowning, unexplained seizures.
Syncope in the setting of exercise is due to cardiac arrhythmia until proven otherwise.
- Structural lesions:
- Valvular and cardiomyopathies: murmurs or signs of CHF require further workup – often need echocardiogram.
- Pulmonary emboli unlikely to present as an isolated syncope given that if there is enough clot burden to obstruct the blood flow, there should be other findings such as SOB, tachycardia, ECG changes.
- Ischemia: Infrequent cause (<3%) and often will have concomitant findings (such as massive STEMI on ECG or classic CP).
Orthostatic
Autonomic system fails to maintain blood pressure with increased heart rate. Often have positional component, such as onset when standing up from sitting position.
- Orthostatic vital signs neither sensitive nor specific and cannot be used in isolation to rule in or out this as cause of syncope.
- Medications: Antihypertensives, diuretics, antidepressants, beta-blockers, alpha-blockers.
- Postprandial hypotension: onset shortly after a meal.
- Intravascular volume loss: dehydration (vomiting, diarrhea, decreased po intake), hemorrhagic (GI, occult trauma, AAA, splenic rupture, retroperitoneal bleeds, etc).
*** SO MAY NOT BE THAT BENIGN AFTER ALL –> thorough exam, including rectal for melena and bedside US for AAA, in appropriate settings and in elderly/high-risk patients
Reflex-mediated
Autonomic system acts inappropriately resulting in reflex bradycardia and vasodilation. Benign cause of syncope with excellent prognosis.
- Vasovagal: prodrome, induced by emotion or pain.
- Situational: cough, micturition, defecation.
- Carotid sinus hypersensitivity: older, male, stimulation of carotid sinus (necktie, shaving, etc).
Neurologic
Transient interruption of blood flow to the brain stem or cerebral cortex.
- Isolated syncope is rare (<1%).
- Routine use of CT head for syncope is not indicated.
- TIA and SAH patients have additional symptoms such as headache (SAH) and/or posterior circulation neurological findings (vertebrobasilar TIA).
- Subclavian steal syndrome – stenotic subclavian artery receives additional blood from the vertebral artery drawing it away from the brainstem. There often will be a difference in the blood pressure in each arm and additional posterior circulation deficits. Patient may report using the affected arm prior to the syncope.
Investigations
ECG
Only mandatory test for all syncope patients.
- Ottawa group found that the patients were at risk for cardiac outcome within 30 days if any of the following were present: (see below related resources)
- Ottawa ECG Criteria3:
- High degree blocks (2nd degree type II or 3rd degree AV)
- Bundle branch + 1st degree block
- RBB + left anterior or posterior block
- Ischemic changes
- Non-sinus rhythm
- Left axis deviation
- ED cardiac monitor abnormalities
- Above ECG criteria likely to under-represent those with rare diagnosis, such as channelopathies, cardiomyopathies, and other inherited arrhythmogenic conditions. Therefore, ECGs (particularly those of younger patients) should be carefully examined for the following abnormalities:
Other Investigations2
- Investigations beyond ECG are required in cases where serious etiology is suspected or where it is not possible to determine the exact cause of syncope based solely on history and physical exam. These may include blood work, CXR, echocardiogram, telemetry, or Holter monitoring. The choice of the investigations is based on the presentation.
Risk Stratification Tools
Most risk stratification rules either have significant limitations or are awaiting validation. The Canadian Syncope Risk Score is currently awaiting validation. Perhaps the most studied is San Francisco Syncope Rule:
San Francisco Syncope Rule Criteria4
Congestive Heart Failure History
Hematocrit < 30%
ECG Abnormal?
Shortness of Breath History
Systolic BP < 90 mmHg at Triage
Important: Pooled sensitivity was 86%. 1.4% of patients who are San Francisco Rule negative will have an adverse event at 7 days. Majority (60%) of missed diagnosis were arrhythmias. Also the rule did not exclude patients for whom the cause of the syncope was obvious, therefore making it unclear if this can be applied to undifferentiated syncope patients1.
Canadian Syncope Risk Score
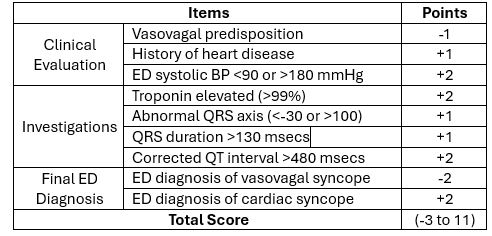

Important: Apply this score when there is a doubt as to potential etiology of syncope. The score predicts adverse events in the next 30 days (versus 7 days in San Francisco Rule). Patients with high score will require further evaluation5.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Approach to the syncope in ED: Based on expert opinion.
Use of the decision rules: Much of the data used in the derivation of the decision rules is retrospective and/or chart reviews. San Francisco Syncope Rule had poor sensitivity of 86% and Canadian Syncope Rule is still awaiting validation.
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Nov 01, 2018
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.