Stevens-Johnson syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) – Treatment
Critical Care / Resuscitation, Ears, Eyes, Nose, and Throat, Inflammatory
Context
- The acute phase of SJS/TEN lasts 8-12 days, with persistent fever, mucous membrane involvement and epidermal sloughing, leaving large, raw painful areas of denuded skin.
- The role of the emergency physician in SJS/TEN treatment involves early detection, withdrawal of offending medications/agents, early consultation with relevant specialists, supportive care and/or ICU/burn unit referral.
- Sterile handling, pain control, and fluid management are simple but effective interventions that can be initiated early.
- Other complications that require monitoring/intervention include electrolyte imbalances, bleeding, evaporative heat loss, hypovolemic shock, insulin resistance, bacteremia from aureus and Pseudomonas, hypercatabolism, and pneumonia.
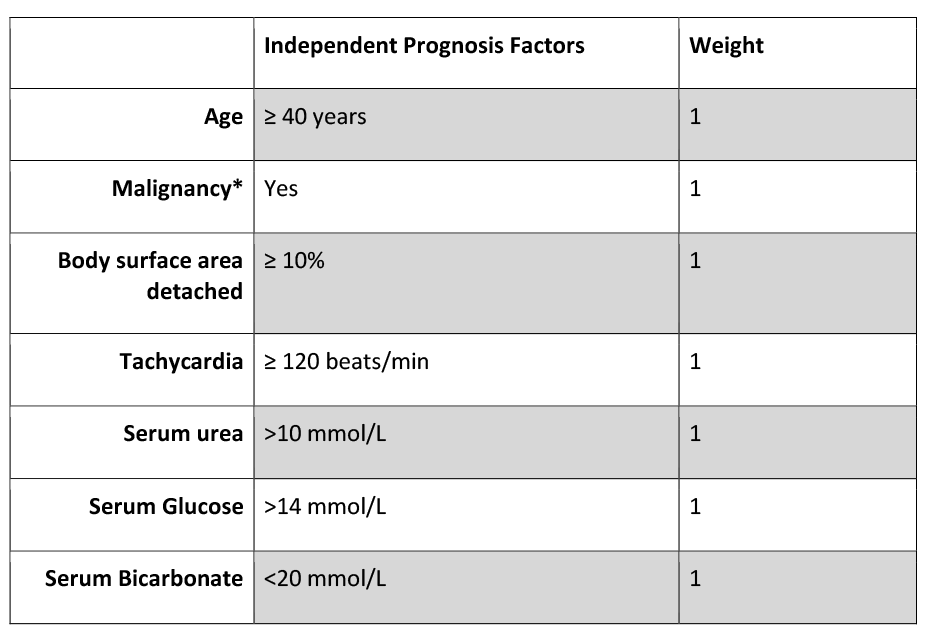
- SCORTEN is a clinical tool that can be used to assess prognosis in patients with SJS/TEN.
There are no definitive treatments recommended for SJS/TEN at this time, however, IVIG/Corticosteroids and Cyclosporine have weak evidence supporting their use.
Recommended Treatment
- Identify any new drugs started within the last 5-56 days (ALDEN tool) and remove the offending agent if possible. Drugs started <5 days ago are unlikely to be the offending agent. Early withdrawal of medication decreases mortality and improves prognosis, especially if done before blister development.
Supportive Management
-
- Pain control
- Mild pain: non-opioid analgesia – Acetaminophen/Ibuprofen.
- Moderate-severe pain: Hydromorphone PO/IV.
- Wound care
- Sterile technique and reverse-isolation precautions.
- Avoid debridement of non-viable epidermis.
- Topical antiseptics such as 0.5% silver nitrate or 0.05% chlorhexidine solution.
- Nutritional support and fluid and electrolyte management as necessary.
- Fluid requirements for SJS/TEN are ~⅔ – ¾ off that of burn patients, give ~2ml/kg X % BSA affected.
- NG tube as needed.
- High calorie requirements.
- Increasing ambient room temperature to 30-32°C to prevent heat loss.
- Prevent, monitor and treat infections/superinfections as sepsis is the leading cause of death in SJS/TEN.
- Routine cultures from skin, blood, gastric tubes and catheters.
- 5% silver nitrate and 0.05% chlorhexidine to paint affected skin areas.
- Monitor and manage vulvovaginal symptoms. If symptomatic:
- Complete pelvic exam.
- Prophylactic vaginal molds.
- Menstrual suppression during the acute phase.
- Intravaginal corticosteroids and topical antifungal agents.
- Ocular Care
- Ophthalmologic consultation.
- Saline rinse and ointment or artificial tears for lubrication.
- Daily topical erythromycin drops
- Conjunctival hyperemia: topical corticosteroids and broad-spectrum antibiotics.
- Pain control
Immunomodulating Treatment (Limited Evidence)
- There are no curative therapeutic interventions known at this time.
- IVIG with short-term, high-dose corticosteroids.
- IVIG 2-3g/kg over 2-3 days.
- Immunosuppressive drugs: Cyclosporine 3-5 mg/kg per day.
Consider
- Mechanical ventilation.
- Phosphate repletion.
- Systemic antibiotics.
- Topical lubricants/steroid drops for acute ocular involvement.
Treatments Not Recommended
- Prophylactic Antibiotics.
- Silver Sulfadiazine.
- Debridement in the Emergency Department without biologic dressings available.
- Systemic corticosteroids – Shown to increase morbidity/mortality through increased risk of sepsis, delayed re-epithelialization and increased protein catabolism.
- IVIG – Increases risk of thrombotic, renal, and hematologic complications, especially in elderly patients or those with cardiovascular and renal comorbidities.
- Thalidomide – TNF-alpha inhibitor, increases mortality.
Criteria For Hospital Admission
- All patients suspected to have SJS/TEN should be admitted to the hospital.
- Admit to ICU or burn unit if SCORTEN ≥ 2, and/or extensive skin detachment or comorbidities.
- The SCORTEN score can be used to prognosticate the severity of disease.
- SCORTEN is calculated based on 7 independent and easily obtainable lab values and has been found to accurately predict mortality.
- Score of 0 or 1 with slow disease progression and limited skin involvement can be treated on non-specialized wards.
- Scores of 2 or higher with more skin involvement or skin detachment >30% of BSA should be treated in the ICU or burn unit and transported to a specialized tertiary centre accordingly.
SCORTEN: Score of toxic epidermal necrolysis.
*Malignancy: includes evolving cancer and hematologic malignancies.
Criteria For Transfer To Another Facility
See above.
Criteria For Close Observation And/or Consult
All suspected cases of SJS/TEN require close observation with consultation to dermatology and other relevant specialists depending on other organs involved (i.e. Gastroenterology, Ophthalmology).
Criteria For Safe Discharge Home
- Ongoing wound care, monitoring for signs of infection (purulent discharge, fevers etc.), adequate pain management including oral care for mucocutaneous lesions are important discharge considerations.
- Patients should return to the ED/hospital if their condition worsens or they develop signs of infection.
- Family and patient education, risk communication, and avoidance of drugs implicated in SJS/TEN.
- Medical alert jewelry.
- Follow up with a family physician to document the resolution of the skin/oral lesions.
- Follow up with a dermatologist within 6 months.
Follow up with relevant specialists depending on organs affected.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
There are no clear treatment guidelines for SJS/TEN due to the lack of large controlled studies and infrequency of SJS/TEN.
There are varying levels of evidence for the use of IVIG, with some studies claiming a benefit of IVIG administration during the early stage of SJS/TEN, in conjunction with IV corticosteroids.
Cyclosporine also requires more research on larger sample sizes. However, in a single centre retrospective review of 71 patients with TEN/SJS, patients who received cyclosporine had a relative mortality benefit compared to IVIG.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Apr 21, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.