Post-Intubation Analgesia and Sedation
Critical Care / Resuscitation
Context
- It is common to neglect post-intubation analgesia and sedation, especially among a multitude of other priorities.
- Rocuronium leads to a delay in post-intubation sedation, compared to its shorter-acting alternative Succinylcholine.
- Under-sedation of ICU patients is associated with an increased duration of mechanical ventilation, and increased the likelihood of delirium with its associated increased ICU stay, mortality, and long-term cognitive impairment.
- Over-sedation also increases risk of delirium.
- Deep sedation within 4 hours of commencing ventilation has been shown to be an independent negative predictor of time to extubation, hospital death, and 180-day mortality.
- Post-intubation Analgesia and Sedation in the ED can have long-lasting consequences and should be treated as an immediate priority after the tube is secured.
Recommended Treatment
Analgesia First
- RSI drugs typically provide minimal analgesia.
- ICU patients treated with analgesia first, and no sedation, had a shorter ICU stay with fewer days on mechanical ventilation.
- Intubation should be immediately followed by an IV bolus of analgesia, particularly if induction was with a sedative (like Propofol) with no analgesic properties.
- Once able, bolus medications can be replaced with an infusion.
Common analgesic options (click image to enlarge):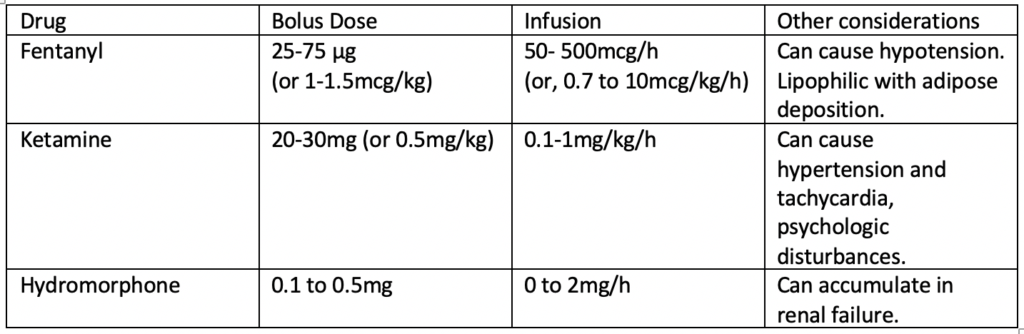
When assessing the adequacy of analgesia, consider using a validated scale like the Behavioural Pain Scale, used for monitoring ICU patients.
- Some of these medications may cause hypotension, so it may be necessary to start a vasopressor infusion to allow for adequate analgesia.
Add Sedation
only once analgesia is addressed:
- Light sedation relieves discomfort, improves synchrony with mechanical ventilation and decreases oxygen requirements and overall work of breathing.
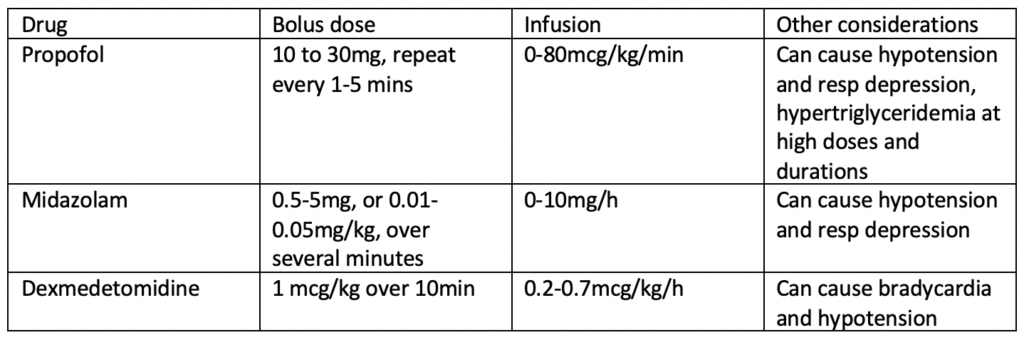
- Benzodiazepines have been associated with longer durations of mechanical ventilation and ICU stays, so are NOT recommended by the Society of Critical Care Medicine (SCCM) and other critical care experts. Short-term boluses may be appropriate, but avoid long-term benzodiazepine infusions.
For any of the drugs below, start with low boluses and titrate up:
- The goal should be to titrate to light sedation, such as -1 to -3 on the Richmond Agitation Sedation Scale below, provided that the patient was able to respond to voice prior to intubation:
Special Scenarios
Hypotension – Medical
- A patient’s low blood pressure should never limit adequate pain control; start and titrate up a vasopressor if necessary. Fentanyl, Ketamine or Midazolam have minimal hypotension.
Hypotension – Trauma
- If this patient has a very low MAP, Ketamine might be a reasonable first choice for its helpful side effect of hypertension and tachycardia.
Delirium Tremens, or Status Epilepticus
- Unlike the typical post-intubation patient, these patients need sedation with GABA agents; use benzodiazepines (BNZ) pre-intubation and add post intubation with a high starting infusion rate. If already on such high doses of BNZ that more are unlikely to help, Propofol is a reasonable next option.
High Intracranial Pressure (ICP)
- Also require heavy sedation, to treat hypertension and limit CNS metabolic demand and rising ICP. Propofol and fentanyl are likely the best first options in these patients.
Pregnancy
- In general, the same strategy as for other critically ill patients.
- Fentanyl for analgesia is appropriate, even if delivery is imminent, to improve maternal hemodynamic stability and reduce risk of awareness, despite risk of fetal/neonatal respiratory depression.
- Ketamine would be appropriate as well.
- Propofol might be considered for low infusion dose post-intubation, due to its short duration, but should ideally be avoided for induction due to higher incidence of hypotension. Evidence is limited.
Treatment Summary
Analgesia first
- Consider Fentanyl 25-50mcg or Ketamine 20-30mg boluses, followed by IV infusion titrated to Behavioural Pain Score BPS.
Add light sedation
- If necessary, and especially if patient is still paralyzed, Propofol or Midazolam bolus or infusion, starting low and titrated to Richmond Agitation Sedation Score RASS.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
In general, evidence for this topic is substantial, including the impact of over- or under-sedation on ICU course. ED-specific evidence is less plentiful, but still of reasonable quality.
Related Information
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Procedural Sedation and AnalgesiaRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 14, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…




POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.