Low Back Pain
Cardinal Presentations / Presenting Problems, Orthopedic
Context
- It is estimated that 70-90% of adults will experience low back pain at some point in their lives. Among the patients presenting in primary care settings 5-10% will have serious underlying pathology (1). The challenge therefore is to rule out serious pathologies without over-investigating.
Diagnostic Process
- Majority of patients will have non-specific mechanical causes of which 90% will recover within 2-4 weeks, with appropriate symptom management (1). These patients only need a history and physical exam to rule out red flags.
- Currently no formal decision rules exist to help to select those patients who do require imaging.
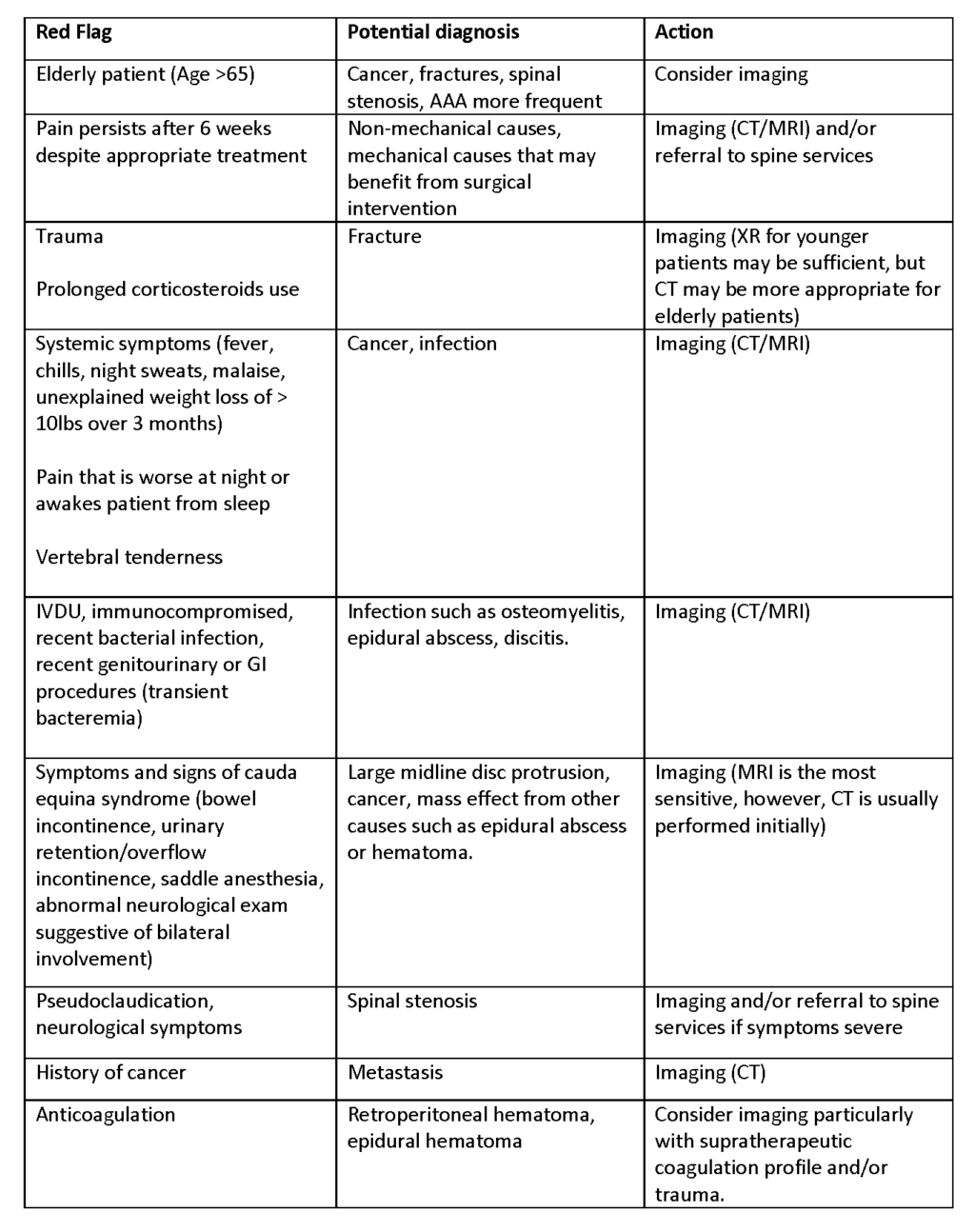
- Historically red flags have been used, although robust evidence for this approach is lacking.
- Red flags such as pain that persists despite appropriate treatment, anticoagulant use, decreased sensation, and nocturnal pain were found predictive of serious outcomes in one retrospective chart review (2), but overall the evidence is poor and the recommendation for the use of red flags is supported primarily by professional guidelines (3, 5).
- Choosing Wisely Canada Campaign in association with Canadian Medical Association and Canadian Association of Emergency Physicians discourage low back spinal imaging in patients with non-traumatic low back pain who have no red flags/pathologic indicators (4).
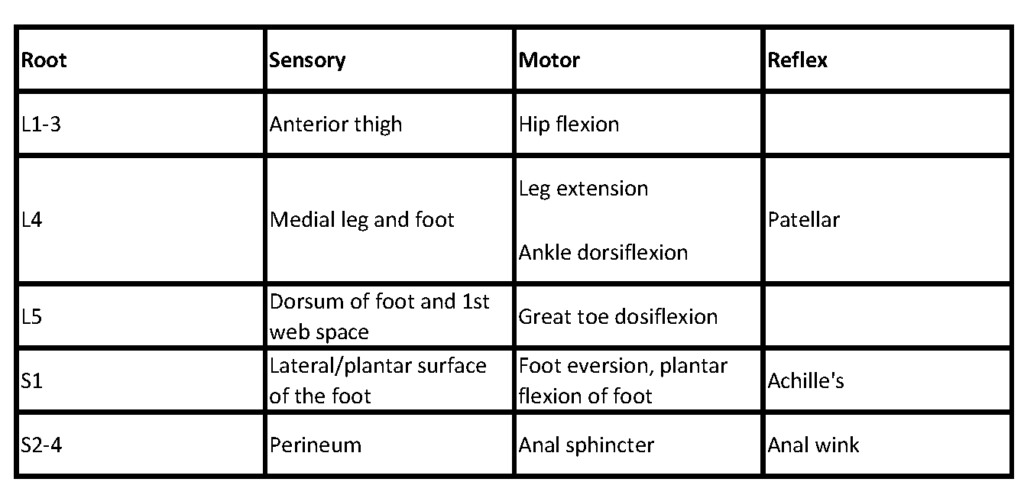
- Patients with neurological involvement suggesting sciatica, who have positive Straight Leg Raise (SLR) test, or who have worsening of pain with Valsalva maneuver are likely to have intervertebral disc protrusion.
- Positive SLR constitutes pain radiating below the knee with ipsilateral hip flexion and/or made worse with dorsiflexion of the ankle while patient is supine. Crossed-leg SLR (reproduction of sciatica when the opposite leg is raised) is insensitive, but highly specific for disc protrusion (1).
- Early imaging in patients WITHOUT red flags is discouraged because radiographic abnormalities are common among asymptomatic adults and bulging discs are frequently incidental findings even in symptomatic patients (1, 6). In addition, the natural history of symptomatic disc protrusion is improvement with only 10% remaining symptomatic at 6 weeks (1). Imaging subjects patients to unnecessary radiation, diagnostic tests, and interventions.
- In patients less than 65 years old non-specific mechanical back pain (sprain/strain) is diagnosed in 70% of cases. Other mechanical causes such as fractures, spinal stenosis, congenital disease, disc pathologies, are found in 17%. One percent of the patients in this age-group will have systemic causes such as cancers, infections, and inflammatory conditions. And 2 % of the patients will have visceral disease such as abdominal aortic aneurysm (AAA), retroperitoneal hematoma, pelvic (i.e. PID, prostatitis), renal (i.e. nephrolithiasis, pyelonephritis), and GI causes (PUD, pancreatitis, cholecystitis).
- In patients older than 65 years neoplasms, fractures, spinal stenosis, and AAA become more frequent. In this group of patients fractures may occur with minimal or no history of trauma.
Common Pitfalls
- Absence of fever does not rule out infection. Sensitivity of fever in the setting of infectious causes of back pain is low. Studies show sensitivity fever is present on only 27-50% of osteomyelitis and 83% of epidural abscess.
- Failure to perform abdominal and respiratory exams may lead to missing other causes that may manifest as back pain. These include pneumonia, cholecystitis, pelvic pathology, pancreatitis, and most importantly AAA. All elderly patients presenting with back pain should undergo point of care ultrasound to rule out AAA.
- Failure to perform a thorough neurological examination may lead to missing important signs of impending surgical emergencies. This is particularly true when patient presents with bilateral neurological symptoms and possible cauda equina. Only patients with neurological complaints and those with suspected cauda equina need a rectal exam.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Use of red flags on history and physical examination
Avoiding early imaging in the patients with low back pain
Related Information
OTHER RELEVANT INFORMATION
Best Case Ever 11: Cauda Equina Syndrome – www.emergencymedicinecases.com
Clinically Organized Relevant Exam (CORE) Back Tool – CFPC
Low Back Pain Exercises – Summit Medical Group
Back Pain Exercises – Saskatchewan Ministry of Health
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 30, 2018
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.