Ischemic Priapism – Treatment
Urological
Context
- Priapism is a pathologic, prolonged penile erection without sexual stimulation, generally lasting longer than four hours.
- It is a urologic emergency requiring treatment in the emergency department and/or urgent urology consultation.
- Short-term, it can cause urinary retention, penile thrombosis, and venous thromboembolism. Long-term sequelae include erectile dysfunction.
Recommended Treatment
Overview of Recommended Treatment Algorithm in the Emergency Department
- Analgesia +/- sedation
- Regional anesthesia
- Minimally invasive technique
- Parenteral antibiotics
- Aspiration-irrigation technique
Endpoints
- Return of bright red blood on aspiration
- Sustained detumescence
Indication
- Ischemic priapism
Contraindication
- Non-ischemic (high flow) priapism
Complications
- Systemic effects of phenylephrine
- Arrythmias
- Angina
- Hypertension
- Reflex bradycardia
- Decreased cardiac output
- Hematoma formation
Treatment Algorithm
- In patients presenting before four hours of sustained erection, attempt conservative interventions like exercise, urination, and ice packs. However, have a low threshold to move on to the next step.
- Place the patient in a monitored unit with continuous cardiac monitoring.
- Provide analgesia +/- sedation with opioids +/- benzodiazepines or ketamine.
- Prep the skin with antiseptic solution (e.g., chlorhexidine) and place a sterile drape.
- Perform a dorsal nerve block +/- ring block to obtain regional anesthesia of the penis:
- Using similar landmarking as above, locate the 10 o’clock and 2 o’clock positions at the base of the penis. Medial to these lay the neurovascular bundles comprising the dorsal arteries and nerves. Both positions will be the injection sites.
- At both the 10 o’clock and 2 o’clock positions at the base of the shaft, puncture the superficial fascia with a 25- to 27-gauge needle, aspirate, and inject 1 to 2 mL of 1% lidocaine without epinephrine. This anesthetizes only the dorsal aspect of the penis.
- To achieve more circumferential anesthesia, perform a ring block. Advance the needle tip laterally toward the 3 o’clock or 9 o’clock position just deep to the superficial fascia. Aspirate and inject local anesthetic as you withdraw. Repeat on the other side.
- Test the block along the penile shaft (not the glans as it is very hard to anesthetize).
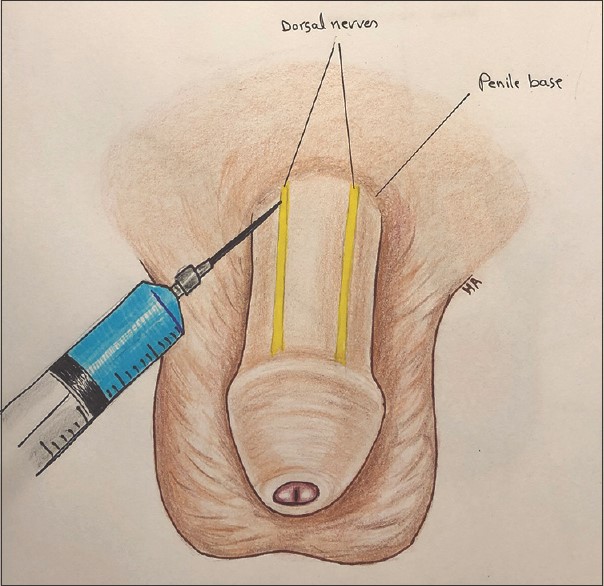
Figure 1. Dorsal Penile Nerve Block
From: Baker A, Patey C, Al-Obaidi H. The occasional low-flow priapism. Can J Rural Med 2020;25:150-3. Accessed August 21, 2022. https://www.cjrm.ca/article.asp?issn=1203-7796;year=2020;volume=25;issue=4;spage=150;epage=153;aulast=Baker
This image is licensed under the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International license.
- Perform the minimally invasive technique of corpora injection with phenylephrine:
- To landmark, go 2 to 4 cm distal to the base of the shaft and locate the dorsal vein of the penis (this is 12 o’clock). Then, locate the 10 o’clock and 2 o’clock positions. One of these will be the injection site (nb: the corpora cavernosa communicate so only one side needs to be injected).
- Using a 25- to 27-gauge needle, puncture the site to a depth of ~0.5 cm and aspirate blood to confirm position in the corpus cavernosum.
- Inject 500 mcg of phenylephrine (1 mL at 500 mcg/mL) into the chosen side.
- Repeat injection q 20 to 30 min (max three injections) until detumescence is achieved. Caution: this is essentially an IV injection so monitor for systemic effects. If this fails, move on to the next step.
- Provide antibiotics IV (e.g., cefazolin).
- Perform the aspiration-irrigation technique:
- Locate the 10 o’clock and 2 o’clock positions 2 to 4 cm from the base of the shaft and palpate the corpora cavernosa (one of these will be the injection site).
- Insert a 19-gauge butterfly needle +/- tubing connected to a 10 to 30 mL syringe into the corpus cavernosum on the chosen side. Advance the needle at a 45-degree angle while applying suction. Once blood is aspirated, stop advancing, stabilize the needle, and obtain a sample to send for blood gas analysis to confirm ischemic priapism.
- Continue aspirating venous blood while milking/massaging the corpora cavernosa to break up clot and changing the syringe as needed. Stop when arterial blood returns or detumescence is achieved; inject 100 to 500 mcg of phenylephrine (0.2 to 1 mL at 500 mcg/mL).
- If aspiration alone fails, irrigate with 20 to 30 mL of cool normal saline (NS), and continue aspirating.
- If detumescence has not been achieved after aspiration and irrigation with NS:
- Inject 100 mcg of phenylephrine (1 mL at 100 mcg/mL) q 3 to 5 min for up to 1 hour (ceiling dose is 1000 mcg) in between aspirations, OR
- Irrigate with diluted phenylephrine at 20 mcg/mL (20 mg of phenylephrine in 1 L of NS).
- Continue cycles of aspiration and irrigation until detumescence is achieved (nb: if injecting phenylephrine here, do not inject the phenylephrine described above at the end of the procedure).
- Remove the needle and apply manual pressure to the injection site and wrap the penis with an elastic bandage to prevent hematoma formation.
Criteria for Consult and Admission
- If detumescence is not achieved or priapism recurs, urology consultation/admission is indicated for consideration of a surgical shunt.
- If the above treatment algorithm achieves sustained detumescence, but the patient required ongoing injections of phenylephrine, admission might be indicated, especially if there is a history of cardiovascular disease.
Criteria for Close Observation and Safe Discharge Home
- If sustained detumescence is achieved, the patient may be safely discharged home after one to two hours of observation (the ideal period is unknown).
- Provide strict return precautions for recurrence.
- Arrange urgent urology follow up.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
This resource is based on moderate quality evidence from the emergency medicine literature, academic texts, and clinical resources. There is variation in the literature on the treatment approach and dosing of phenylephrine.
Related Information
Reference List
Davis JE and Silverman MA. Urologic Procedures. In: Chanmugam AS, Chudnofsky CR, DeBlieux PMC, Mattu A, Swadron SP, Winters ME. eds. Roberts and Hedges’ Clinical Procedures in Emergency Medicine and Acute Care, 7e. Elsevier; 2019. Accessed July 28, 2022. https://www.clinicalkey.com/#!/content/book/3-s2.0-B9780323354783000555
Boswell B and Thomas AA. Pediatric Genitourinary and Renal Tract Disorders. In: Walls RM, Hockberger RS, Gausche-Hill M, Erickson TB, Wilcox SR. eds. Rosen’s Emergency Medicine: Concepts and Clinical Practice, 10e. Elsevier; 2023. Accessed July 28, 2022. https://www.clinicalkey.com/#!/content/book/3-s2.0-B9780323757898001687
Davis JE. Male Genital Problems. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw Hill; 2020. Accessed July 28, 2022. https://accessmedicine.mhmedical.com/content.aspx?bookid=2353§ionid=219643185
Mason J. Priapism Reduction. EM:RAP HD. July, 2022. Accessed July 28, 2022. https://www.emrap.org/hd/playlist/latest/chapter/priapism/priapism
Deveci S. Priapism. In: O’Leary MP and Hockberger RS. eds. UpToDate. Waltham, MA. Accessed July 28, 2022. https://www.uptodate.com/contents/priapism?search=priapism&source=search_result&selectedTitle=1~61&usage_type=default&display_rank=1#H16
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Aug 22, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.