Exertional Heat Illness
Environmental Injuries / Exposures
Context
- Exertional heat illness (EHI) is the leading cause of morbidity and mortality among young athletes in North America.
- Other subgroups who exert themselves in or around heat (e.g. firefighters, soldiers, and outdoor labourers) are also at increased risk of EHI.
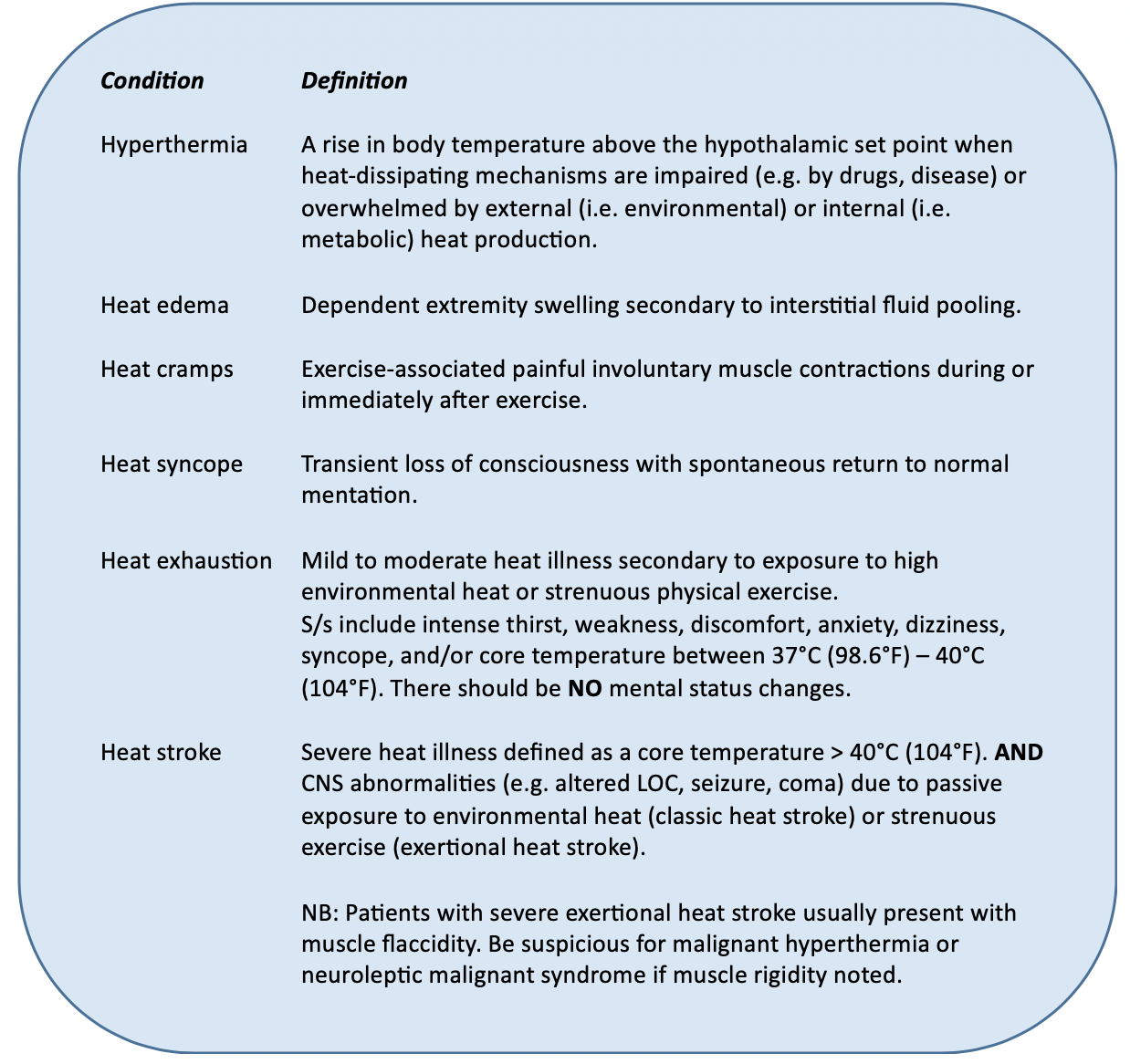
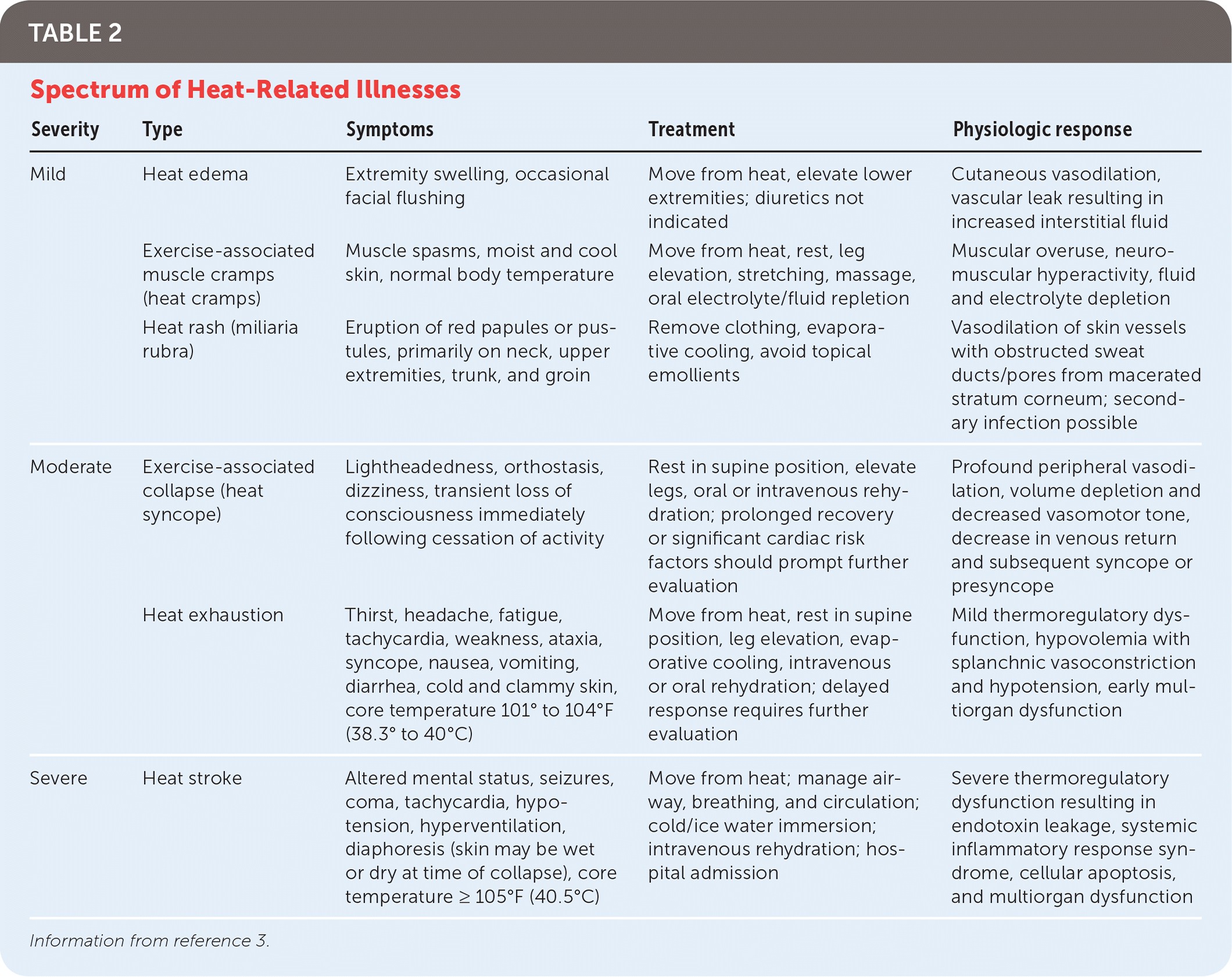
- EHI manifests via a spectrum of disease from minor (e.g. heat cramps) to severe (e.g. heat stroke):
- While the pathophysiology of EHI is largely unclear, morbidity and mortality are a direct result of ischemia and oxidative and nitrosative stress. This leads to a culmination of thermoregulatory failure, heat stroke, and circulatory shock.
- Quick recognition and management are crucial as prognosis is worse when cooling is delayed and the core temperature is allowed to remain above the critical threshold of 40.5 to 41.0°C (105 to 106°F) for any period of time.
Recommended Treatment
Management
- Remove from heat source.
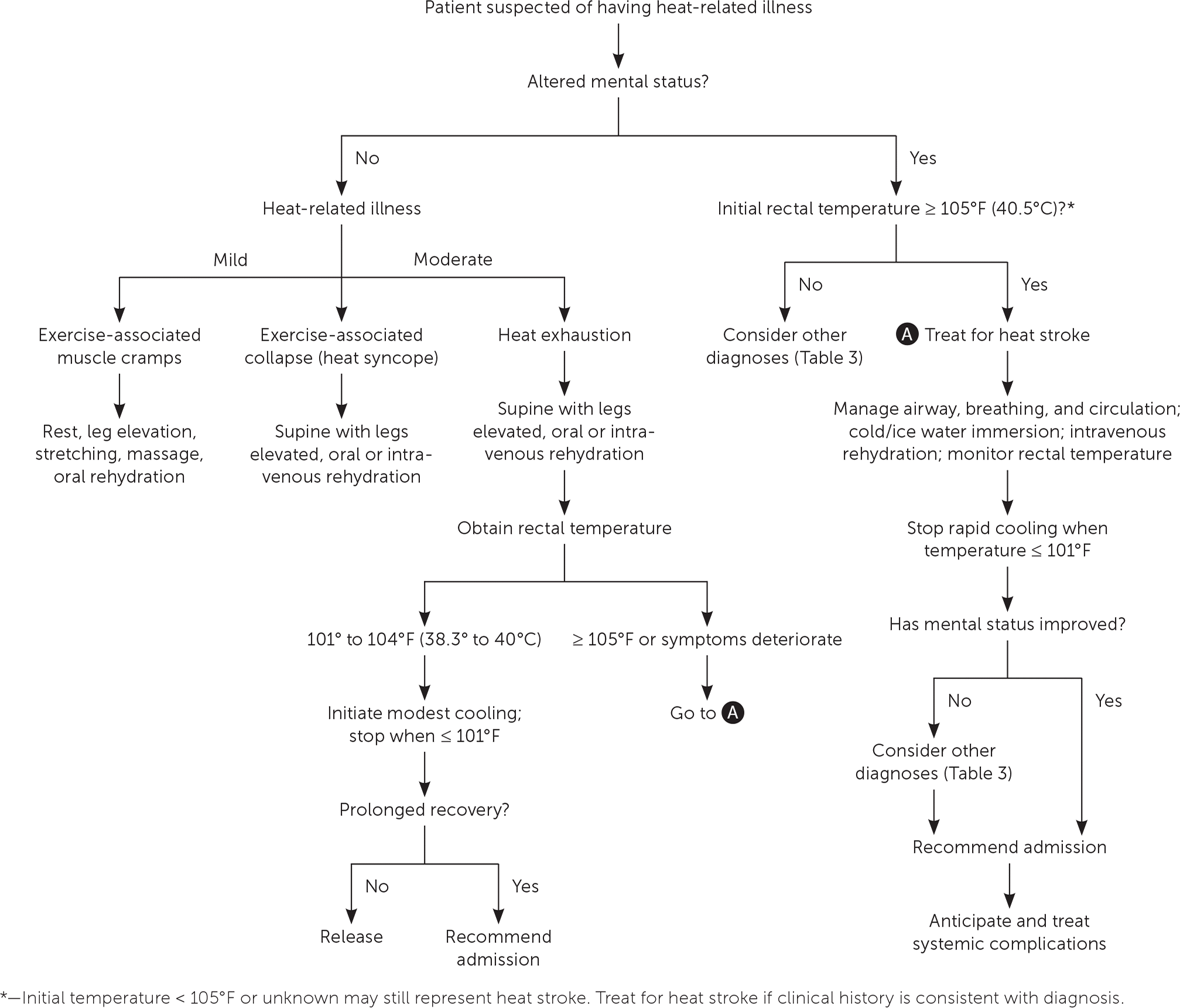
- Initial assessment (e.g. ABCs, vitals, rectal temperature).
- Large bore IV access, supplemental oxygen if needed, cardia telemetry.
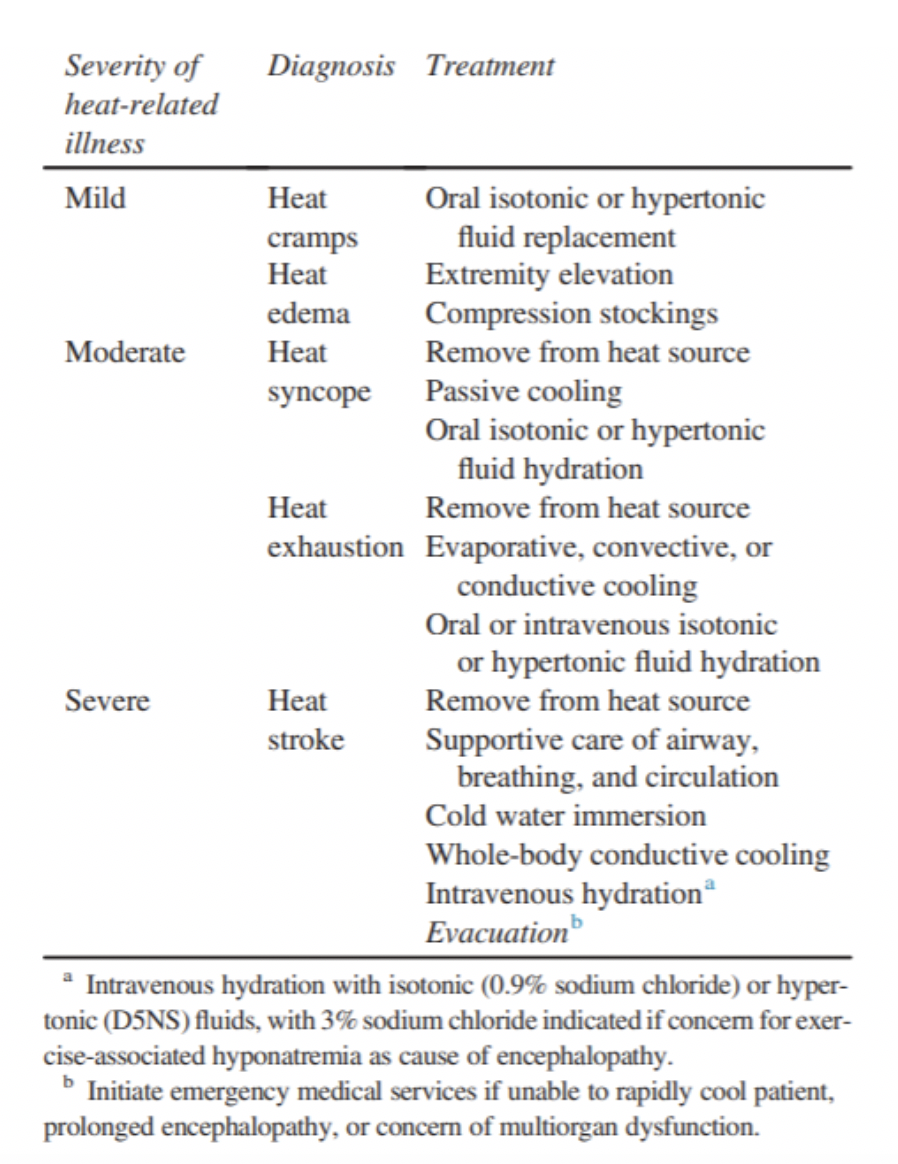
- For mild heat illness (e.g. heat cramps), provide oral fluid replacement.
- For moderate heat illness (e.g. heat syncope, heat exhaustion), provide oral IV fluids and initiate cooling measures (see below).
- Severe heat illness (e.g. heat stroke), rapidly cool (within 30 minutes) initiate cooling measures including ice bath immersion (see below).
- Consider benzodiazepines to manage agitation and shivering.
- Cooling Methods:
- Should be initiated as soon as possible.
- Remove all clothing/equipment.
- If performing cold water immersion, ideally immerse as much of the body as safely possible in ice water with temperature between 2 to 15°C (35 to 60°F) and stir the water vigorously during cooling.
- Ensure rectal thermometer is in place for continuous measurement.
- Continue cooling until the patient’s rectal temperature reaches 39°C (102°F).
- If ice water immersion is not feasible, cool the patient using the best available means such as:
- Placing patient in a cold shower.
- Dousing them with cold water and facilitate cooling with fans.
- Moving them to a cool shaded area and applying cold wet towels to as much of the body surface as possible.
- Placing wet ice packs all over the body, especially over skin covering major vessels (e.g. groin, axilla).
- Placing chemical cold packs over cheeks, palms, and soles.
Source: Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Heat Illness: 2019 Update.
- Reassess (e.g. vitals, rectal temperature, urine output, cardiac telemetry).
- Order relevant bloodwork given the clinical context. (e.g. electrolytes, liver function, cardiac biomarkers, creatine kinase, ECG).
- Supportive measures (e.g. cooling, fluid resuscitation, correct electrolyte disturbances).
- No role for pharmacologic therapy (e.g. acetaminophen) in exertional heat stroke.
Criteria For Hospital Admission
Patients suspected to have a severe heat illness (i.e. heat stroke) and/or signs of hemodynamic instability should be admitted for a period of observation and monitoring for complications.
Criteria For Transfer To Another Facility
Dependent on local guidelines.
Criteria For Close Observation And/or Consult
Will depend on clinical presentation and patient’s progress during hospitalization. Relevant specialties may be required depending on the nature of the patient’s complication (e.g. internal medicine for acute kidney injury).
Criteria For Safe Discharge Home
- Will depend on clinical presentation and patient’s progress during hospitalization.
- For healthy patients at baseline who recover rapidly from exertional heat stroke with cooling and have no residual symptoms, common practice at many major endurance events involves discharge after observation for up to six-hours. This also includes a thorough reexamination prior to discharge and arrangements made for appropriate follow-up (e.g. family physician).
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Cold water immersion is the optimal cooling method for heat stroke.
- Target temperature for cooling heat stroke patients should be not be less than 39°C.
- Rectal temperature is the most accurate measurement of core hyperthermia compared to axillary, oral, or aural thermometry.
- Cold intravenous fluids (4°C) should be used adjunctively in cooling heat stroke patients.
- Evaporative or convective cooling can be considered as adjunct cooling methods if cold water immersion is unavailable.
- Dehydration should be minimized in heat illness.
- Ice packs should be applied to cover the entire body.
- Antipyretics should be avoided in heat illness.
- There is currently no role for routine treatment of exertional heat stroke with dantrolene.
Related Information
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Mar 23, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.