Deep Vein Thrombosis – Diagnosis
Cardiovascular, Hematological / Oncological
Context
- Deep vein thrombosis (DVT) is common, with over 45,000 cases diagnosed in Canada each year.
- Complications can include pulmonary embolism (PE) and post-thrombotic syndrome.
- Risk factors for development of a DVT are closely related to Virchow’s triad (venous stasis, vascular injury and hypercoagulability) including recent surgery, immobilization, malignancy, trauma, pregnancy, estrogen use, and varicose veins.
- Patients may present with calf pain or cramping, warmth, erythema and edema to a unilateral limb, primarily the lower limb.
- 4-10% of DVT’s involve upper extremity:
- 80% of these are secondary:
- Pacemaker or Central Venous Catheters (including peripherally inserted central catheters (PICC line).
- Anatomical: cervical rib; hypertrophy of scalenus muscle.
- Trauma: clavicle fracture.
- Paget-Schroetter syndrome:
- Venous thrombosis of the subclavian vein in thoracic inlet syndrome.
- Typically, young athletes.
- Sports like baseball, swimming, or tennis.
- Cancer
- Pancoast tumor.
- 80% of these are secondary:
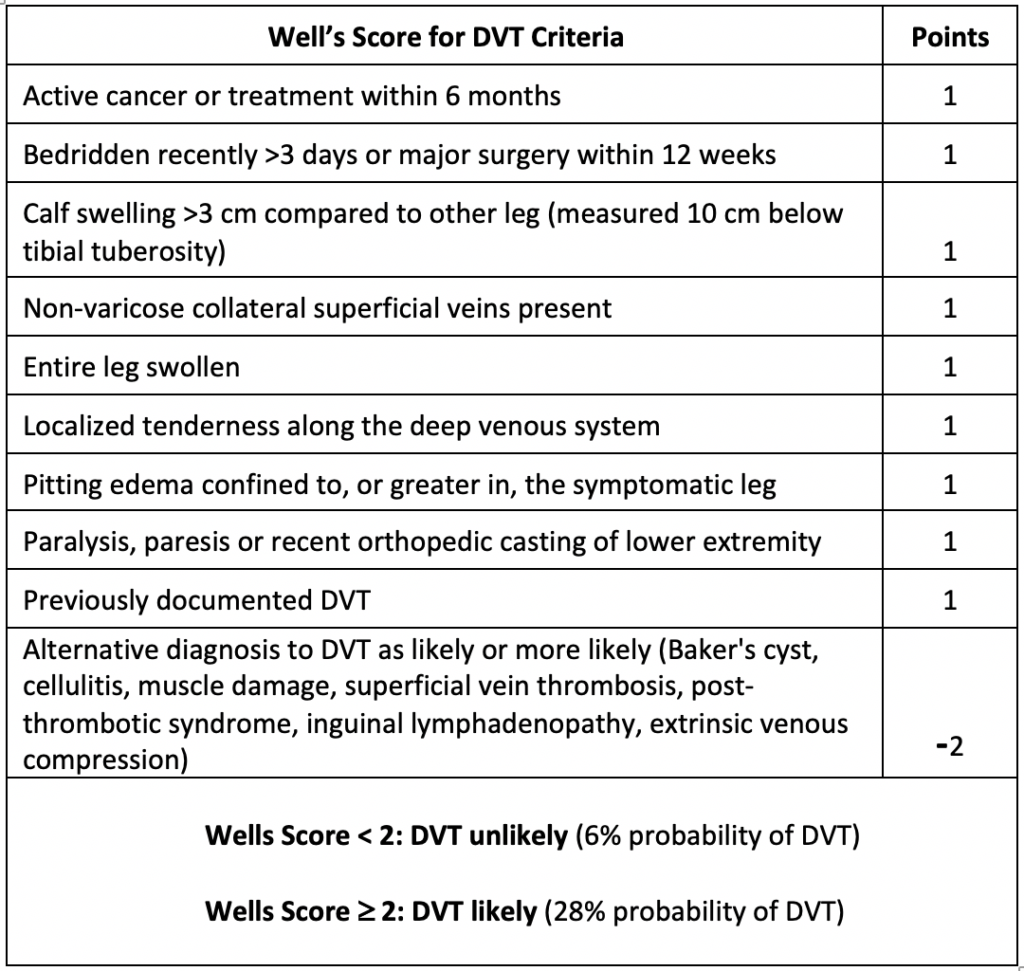
- Diagnosis of DVT requires determining the pre-test probability of DVT either through clinical gestalt (depends on clinical experience) or better to use a clinical tool, such as the Well’s Score followed by D-dimer/ultrasound as indicated.
Diagnostic Process
- Thrombosis Canada recommends patients presenting with suspected DVT should be risk stratified. The most commonly used tool is the Well’s Score for DVT.
- Wells Score > 2: DVT Likely
- Perform Venous Compression Ultrasound (CUS) of the extremity
- CUS is positive, initiate appropriate treatment for DVT.
- CUS is negative, recommend performing a D-Dimer:
- D-Dimer is negative, DVT can be ruled out.
- D-Dimer is positive, repeat CUS in one week.
- Perform Venous Compression Ultrasound (CUS) of the extremity
- Wells Score < 2: DVT Unlikely
- Perform a D-Dimer:
- D-Dimer is negative, a DVT can be ruled out.
- D-Dimer is positive, perform a CUS.
- If the CUS is positive, a diagnosis of DVT can be made.
- If the CUS is negative, DVT can be ruled out.
- Perform a D-Dimer:
- D-Dimer
- D-Dimer is a marker of fibrin clot breakdown.
- It is a highly sensitive (up to 90%) but non-specific test.
- D-dimer can be elevated in many other conditions including:
- Inflammatory diseases.
- Infection.
- Malignancy.
- Advanced age – the use of an age-adjusted D-dimer cutoff has not been well validated for excluding DVT (unlike for PE). As such, its use for DVT diagnosis is not routinely recommended at this time by Thrombosis Canada.
- Pregnancy.
- Trauma.
- Surgery.
- In contrast to PE, there is no evidence to suggest that an age-adjusted D-dimer cutoff should be used to exclude DVT.
- A D-dimer less than a fixed cut-off, in combination with validated clinical prediction rules (Wells score) can be used to rule out DVT in patients where DVT is deemed unlikely.
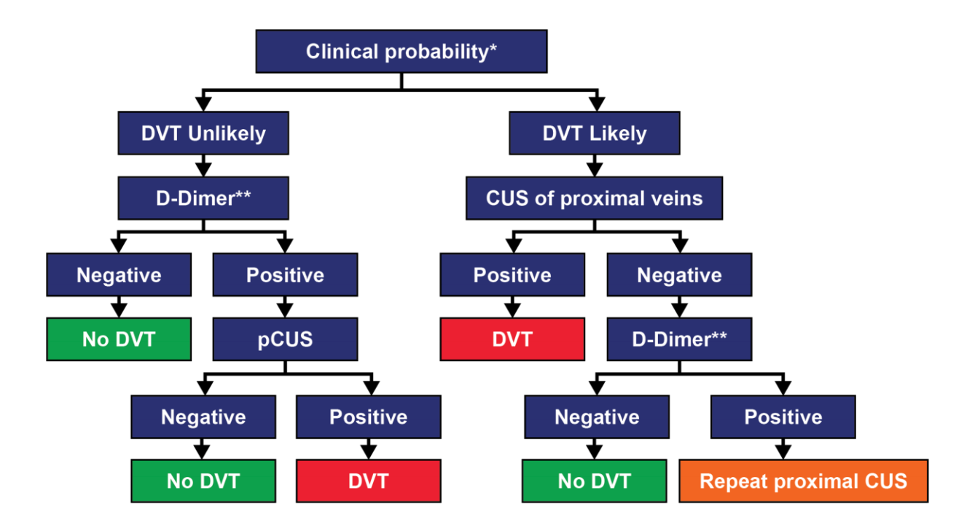
Source: Diagnostic strategy adapted from Thrombosis Canada Deep Vein Thrombosis Diagnosis guideline.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
This diagnostic strategy has been approved and developed by Thrombosis Canada.
Related Information
Reference List
Relevant Resources

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Nov 23, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.