1st Trimester Bleeding: Miscarriage – Treatment
Obstetrics and Gynecology
Context
- Early Pregnancy Loss (EPL): Intrauterine pregnancy (IUP) loss < 20 weeks Gestational Age (GA).
- 80% occur in first 12 weeks GA.
- 15-25% of all pregnancies.
Recommended Treatment
Overall treatment principles:
- Hemodynamic stabilization.
- Prevent alloimmunization if Rh negative.
- Guidance and pain control.
- If nonviable – expectant, medical, or surgical management usually OB/GYN input.
A) Initial ED treatment (threatened, inevitable, incomplete, missed, and completed miscarriages):
- Treat complications:
- Infection (endometritis and/or septic abortion) occurs in 2-3% of cases, irrespective of treatment.
- Hemorrhage
- Retained Products of Conception
- OB/GYN consult, admission, fluid resuscitation, antibiotics
- Prevent Rh alloimmunization:
- For Rh Negative patients, administer:
- If < 12 weeks GA:
- 50-120 mcg anti-D immunoglobulin within 72 hours (expectant, medical or surgical management).
- 300 mcg dose is acceptable.
- If >12 weeks GA: dose = 300 mcg IM.
- Symptom management:
- Naproxen 500 mg q12h or Ibuprofen 800 mg q8h
- Acetaminophen 1000 mg q6h
- Heating pads
- Consider antiemetics, especially if receiving medical management with misoprostol
- Address psychological concerns:
- Acknowledge distress and grief
- Reassure that they are not at fault
- Reassure that they are not at increased risk of future miscarriages. Fewer than 5% of women will experience two miscarriages, and only 1% experience three or more.
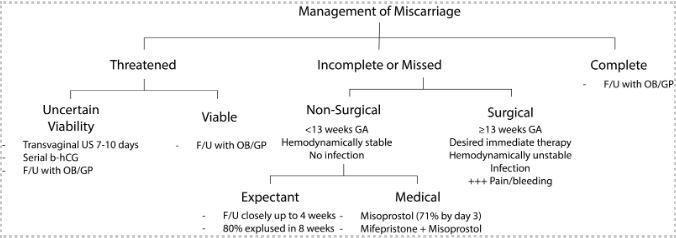
B) Treatment by Miscarriage Category:
Incomplete, inevitable or missed miscarriage:
- Consider OB/GYN consult to discuss surgical, medical, and expectant options.
- The MIST trial found no difference in rates of infection between all three options, but an increased rate of unplanned admissions and surgical management with expectant and medical management.
- If available F/U with OB/GYN for monitoring of miscarriage completion through expectant, medical, or surgical management often best.
Created by Ella Barrett-Chan, MSI UBC 2023
Threatened Miscarriage:
- Viability confirmed: Return care to main OB provider.
- Viability uncertain: see PECS Miscarriage – Diagnosis.
- Provide anticipatory guidance on possibility of future miscarriage.
Completed Miscarriage:
- F/U with primary OB provider (or Early Pregnancy Assessment Clinic if in the Lower Mainland) to ensure resolution of bleeding (< 72 hours).
C) Discharge planning:
- Discharge Instructions: Return to ED if: significant increase in bleeding, pain, lightheadedness or fainting, fever, foul-smelling discharge.
- F/U with main OB provider within 72 hours.
Counselling:
Lower Mainland Resources for follow up:
- For TVUS, miscarriage management, grief/loss counselling, <13 weeks GA
- Early Pregnancy Assessment Clinic at BC Women’s Hospital
- Early Pregnancy Assessment Clinic at Surrey Memorial Hospital
- If a patient has had two or more losses:
Criteria For Safe Discharge Home
- Bleeding controlled and hemodynamically stable.
- No infection – septic miscarriage (no fever, uterine tenderness, leukocytosis, foul-smelling discharge).
- Follow up arranged.
- Discharge counselling and instructions completed.
Criteria For Hospital Admission
Requiring urgent surgical management:
- Heavy bleeding and/or hemodynamic instability.
- Septic miscarriage.
Criteria For Close Observation And/or Consult
OB/GYN consult if:
- Hemodynamic instability.
- Septic miscarriage.
- Incomplete, inevitable, or missed miscarriage for discussion of expectant vs. medical vs. surgical management and arrangement of timely follow up.
- Unclear diagnosis of complete vs. incomplete miscarriage.
Criteria For Transfer To Another Facility
Indications: Anticipating surgical management not available at current facility.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Comparison of expectant vs. medical vs. surgical management.
All women with 1st trimester miscarriage who are Rh negative should receive Rho-gam5. Based on expert opinion and extrapolation.
Resources
Clinical Resources:
- Discharge teaching for patients with early pregnancy loss:
- Miscarriage and Bleeding in Early Pregnancy Patient Information Sheet.
- Discharge instructions: Threatened miscarriage Video (YouTube: Sunnybrook Hospital).
- Discharge Teaching for Patients Experiencing an Early Pregnancy Loss (Provincial Council for Maternal and Child Health).
- Patient resource comparing expectant, medical, and surgical management (BC Women’s Early Pregnancy Assessment Clinic).
Additional topic reviews:
- Miscarriage – Diagnosis PECS.
- EM Rounds Blog (St John’s Hospital) on early pregnancy and PUL.
- Emergency Medicine Cases blog and podcast on early pregnancy complications.
- Breaking Bad News (Provincial Council for Maternal and Child Health).
- Communicating with Families Experiencing Pregnancy Loss (Provincial Council for Maternal and Child Health).
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 05, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.